Relatively poor compensation compared to other specialties threatens the future of the infectious diseases workforce.
ID physicians bill for most of their services using evaluation and management codes, which are selected according to criteria defined by the Centers for Medicare and Medicaid Services and the American Medical Association’s Current Procedural Terminology. While these criteria are well-defined, variable coding for similar services may occur among ID physicians, perhaps due to unfamiliarity with billing rules or concerns for overbilling relative to peers.
Understanding nationwide billing practices may help improve ID compensation by empowering ID physicians to select more appropriate levels of service for their complex and valuable work.
A look at the data
To better understand ID billing practices, I reviewed inpatient Medicare code selections by ID physicians over a 14-year period from publicly-available CMS data and compared these selections to billing by hospitalists and internists. All charges to Medicare using CPT codes for initial inpatient care (99221, 99222 and 99223) and subsequent inpatient care (99231, 99232 and 99233) for these specialties from 2011 through 2024 were reviewed.
Because CMS did not recognize hospital medicine as a separate specialty until 2017, services by hospitalists and internists were counted together.
For the analysis, I reviewed 531,505,451 inpatient Medicare charges from 2011 to 2024, consisting of 12,760,853 initial and 57,259,193 subsequent ID visits and 80,238,041 initial and 381,247,364 subsequent visits by internists and hospitalists
Initial and subsequent ID visits
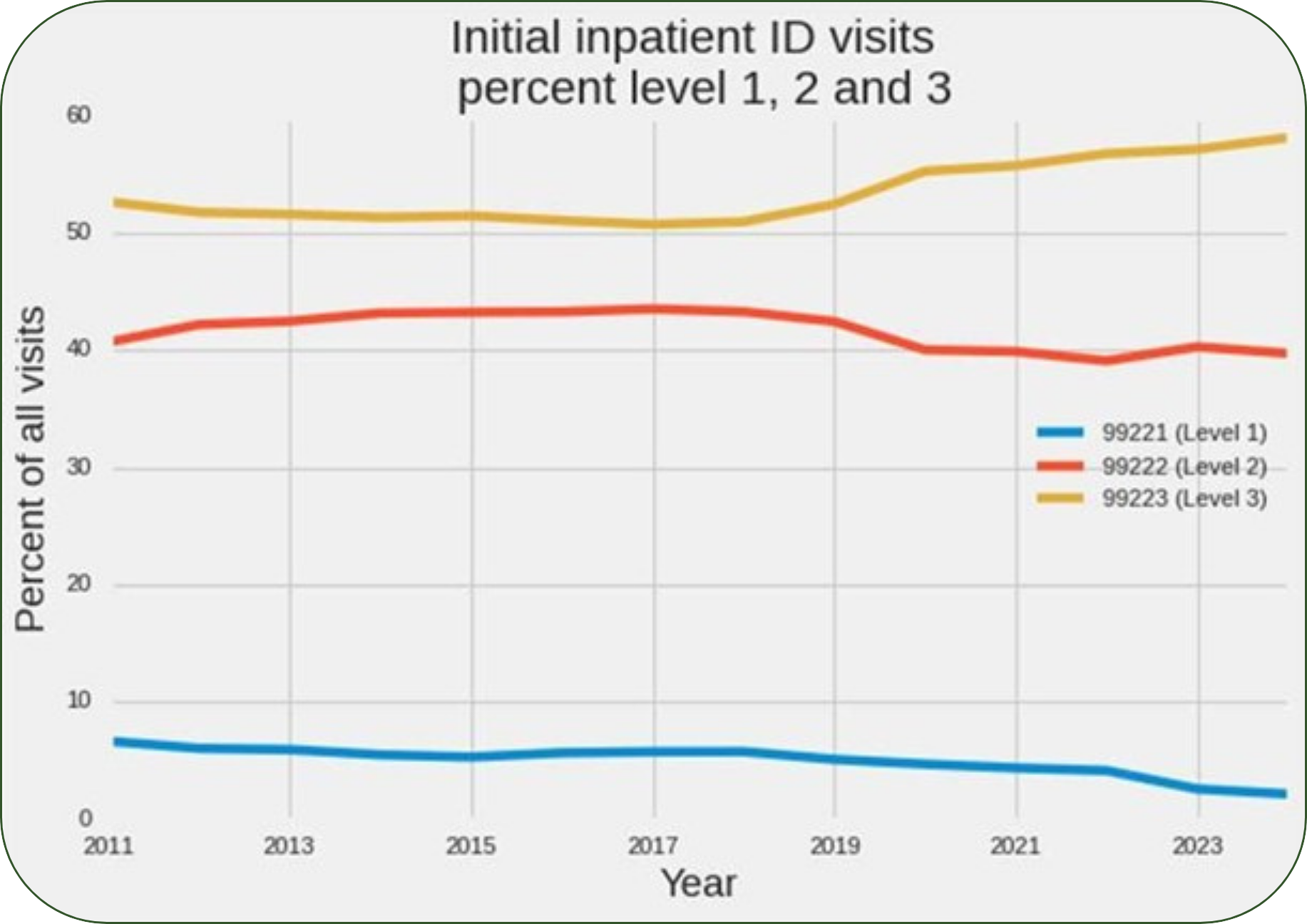
Among initial inpatient ID visits, 53% were billed at level 3 (99223), 42% were level 2 (99222), and 5% were level 1 (99221). The use of code 99223 became more common over time, with 99223 accounting for 53% of new visits in 2011 and 58% of new visits in 2024.
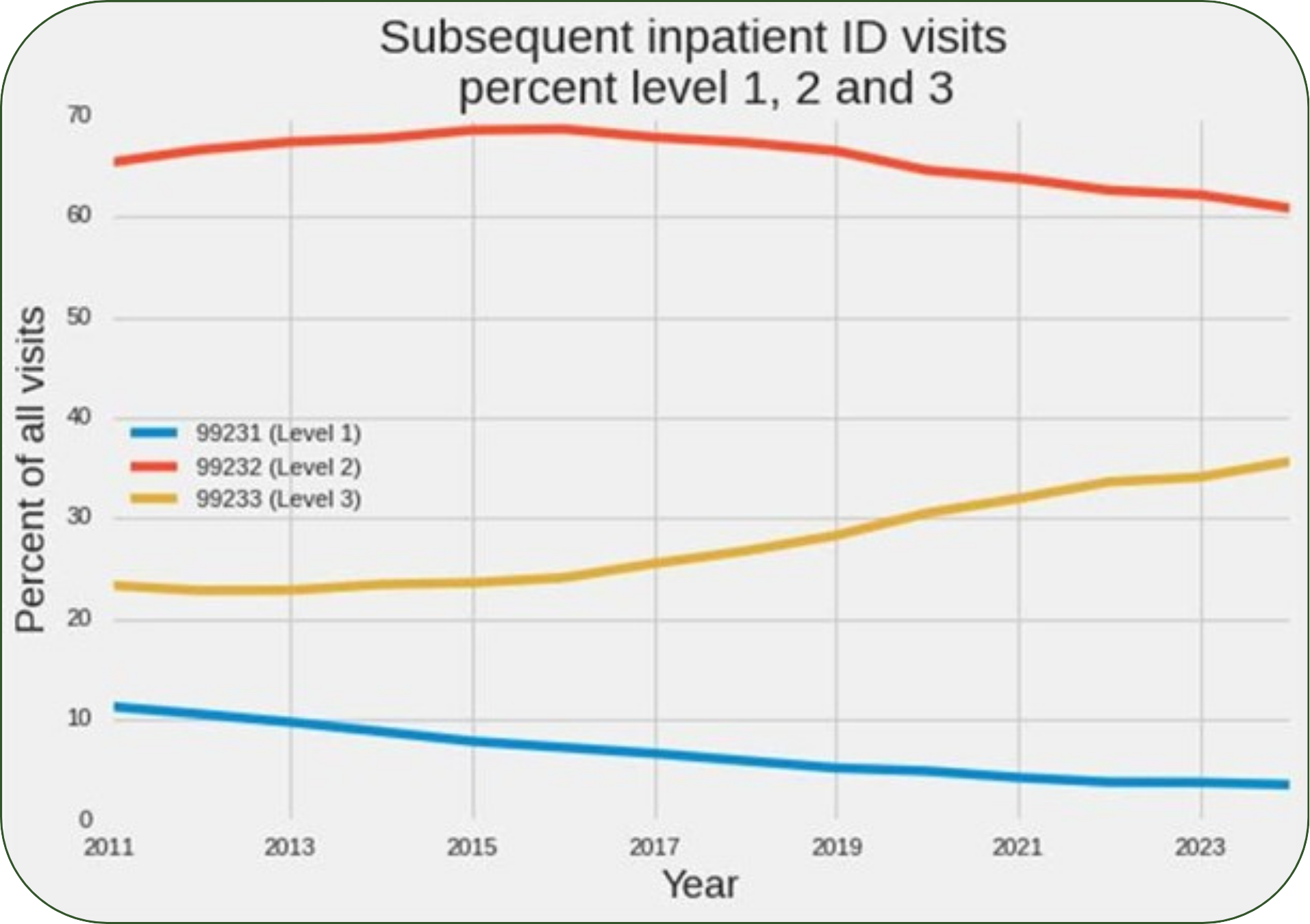
Of subsequent ID visits, 27% were Level 3 (99233), 66% were Level 2 (99232), and 7% were Level 1 (99231). The percentage of subsequent visits billed as level 3 also increased over the 14-year period, rising from 23% in 2011 to 36% in 2024.
ID versus hospitalists and internists
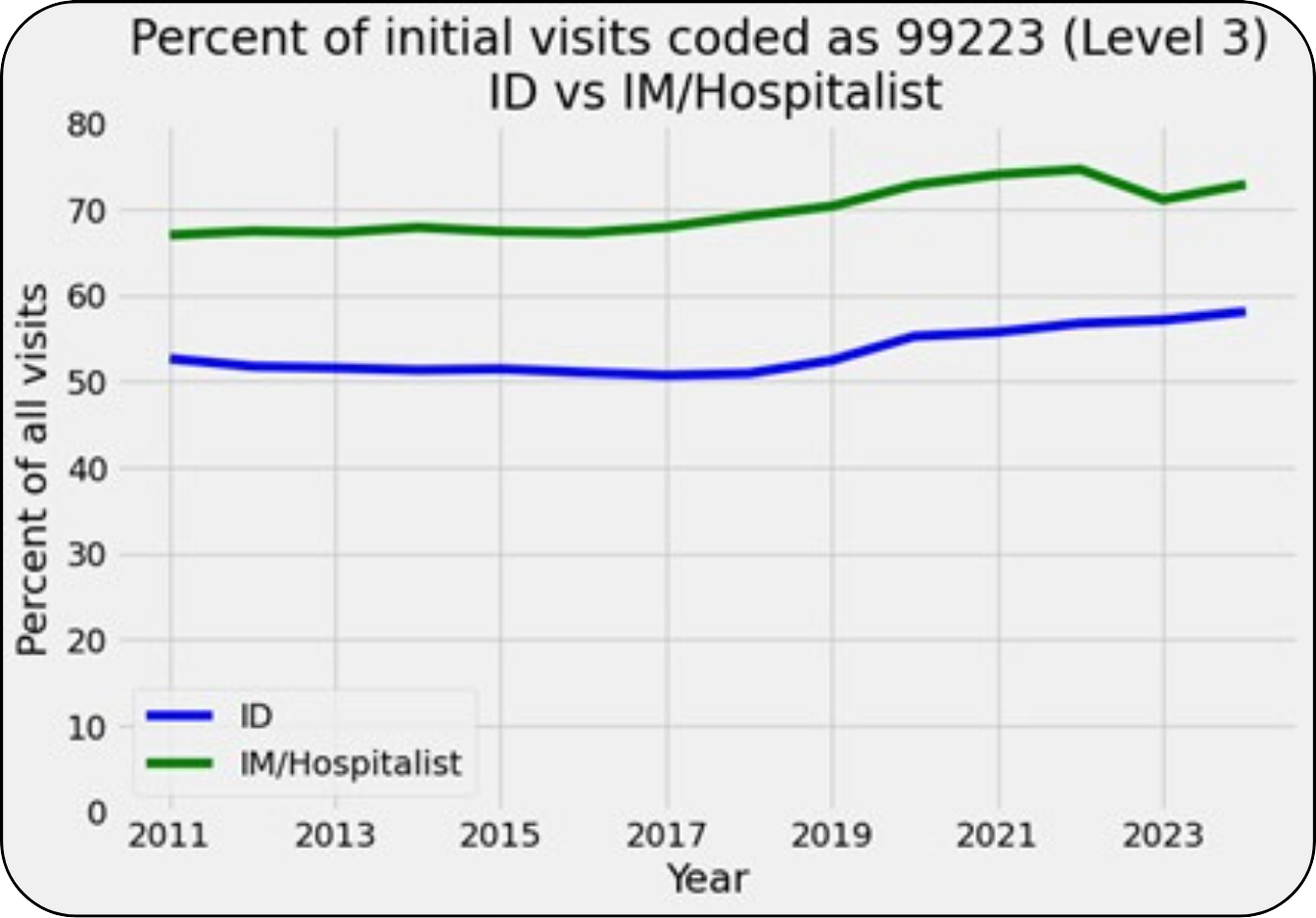
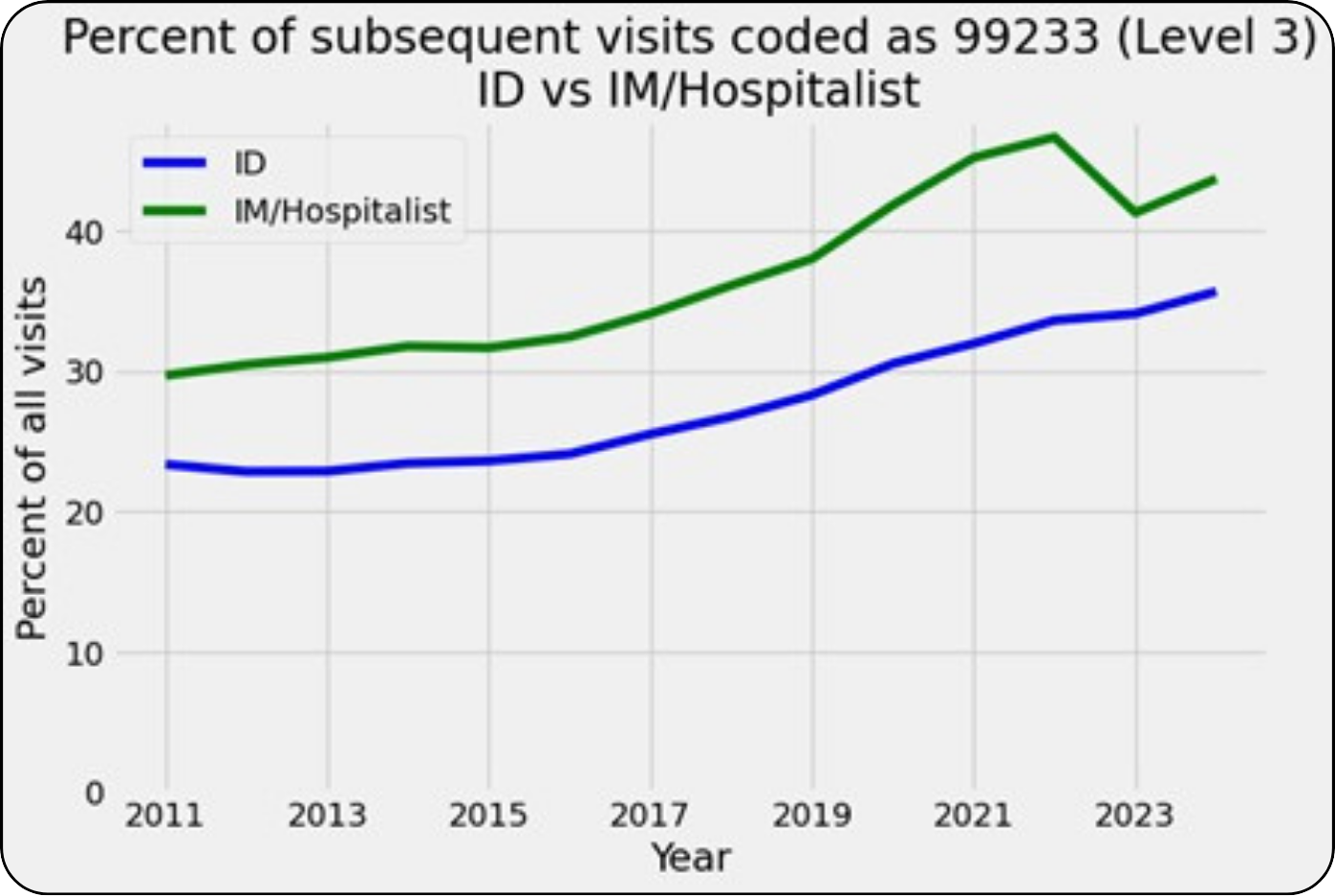
Of the initial visits by internists and hospitalists, 70% were level 3, 26% were level 2, and 4% were level 1. Of subsequent visits by internists and hospitalists, 36% were level 3, 58% were level 2, and 6% were level 1.
Compared to ID physicians, internists and hospitalists were more likely to select a level 3 code (99223) for an initial visit and to select a level 3 code (99233) for a subsequent visit. Although the use of level 3 codes by ID physicians became more common over the 14-year period reviewed, use of these codes by internists and hospitalists followed a similar trend.
Lessons for ID physicians
These data show that ID physicians, internists and hospitalists typically bill at the highest level for an initial inpatient visit, while they most often select the level 2 E/M code for a subsequent visit, and they rarely use level 1 codes.
While the most common E/M code selections were similar among ID physicians, internists and hospitalists, ID physicians were less likely to select a level 3 code for initial and subsequent visits. The use of level 3 billing by ID physicians increased over time, which may represent increasing complexity and severity of illness among ID inpatients, or increasing awareness of appropriate billing practices by ID physicians. A similar trend was observed among internists and hospitalists.
The criteria for E/M code selection were updated in 2023 to simplify the billing process and reduce the documentation burden for physicians. Those changes resulted in less emphasis on the number of problems managed and more emphasis on complexity, risk and data reviewed as well as expanded criteria for time-based billing.
These updates might therefore be expected to result in higher-level code selection among ID physicians, who are often tasked with managing a single, complex problem and reviewing extensive data.
However, while the use of level 3 billing rose over the 14-year period reviewed, there was not a major change after 2023, and level 3 code selection remains significantly lower among ID physicians compared to internists and hospitalists. This might represent a missed opportunity for ID physicians providing complex care to improve their relatively low compensation.
This review is limited by only including Medicare charges and by the exclusion of other billing codes, including critical care billing, prolonged service codes and the ID add-on code G0545, which was introduced in 2025. Additionally, it was not possible to determine if billing code selections were correctly supported by the care provided and by clinical documentation.
Despite these limitations, these data may help inform ID physicians on their billing practices relative to their ID peers, and relative to hospitalists and internists. Ultimately this may help ID physicians to consider more accurate code selections and to bill appropriately for their complex and valuable care.
The Coding Corner updates IDSA members about coding and billing issues. If you would like to ask a question for the Coding Corner, or if you have a general coding and billing question, please visit the Coding and Payment page and click on the yellow “Ask the Coder” button at the bottom of the page (member login required to submit a question).
