Looking back: Managing our first campus outbreak of COVID-19
Facebook Twitter LinkedIn EmailAs we were writing this post, several outbreaks on college and university campuses were capturing the headlines and causing schools to shut down their campuses and switch to online final exams just before students and their faculty headed off for their winter break. In our previous post on this blog, we described the essential policies and practices we employed to detect and prevent the spread of COVID-19 on Dartmouth’s campus earlier in the pandemic.
Our combined use of pre-arrival testing, regular on-campus PCR and rapid antigen testing, an indoor mask mandate, reduced occupancy in the dormitories, and spaced seating in classrooms and dining halls proved successful at minimizing the spread of SARS- CoV-2. Then, just as vaccines were being rolled out, and before we had the benefits of their protection, we faced our first COVID-19 outbreak within our student population that would test our containment capabilities and emergency response plans.
Initial cases and stepwise safety measures
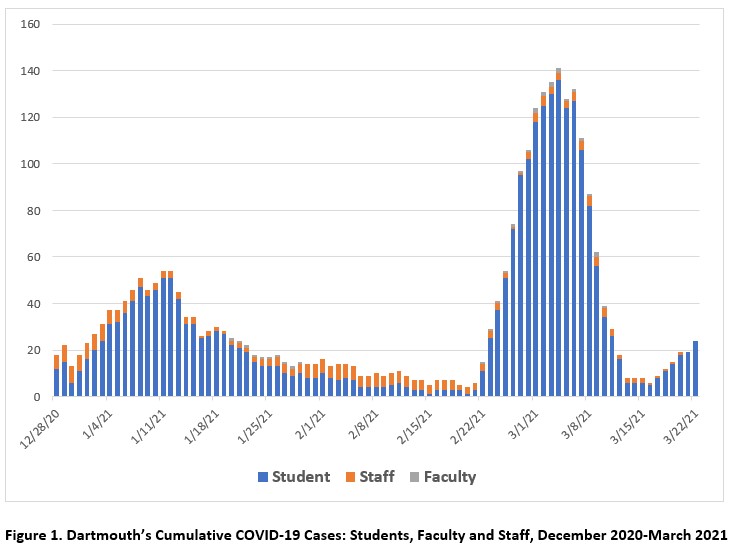
It began simply enough with a small, rather unremarkable uptick in positive tests among our students on a Monday in late February 2021. It was only 11 cases, and while we had enjoyed single digit case numbers for the past month, this initial report did not immediately sound any alarms. But with our college health services team monitoring results in real time, they alerted our COVID-19 Task Force’s Core Group as they saw more positive results rolling in throughout the day. By the next morning, the number of cases jumped to 25 and continued to multiply by a factor of 1.5-2 over the next few days (see Figure 1). I recall being in our COVID-19 Health and Epidemiology meetings in those early days where my colleagues provided live updates every few minutes – and I distinctly recall how unnerving it was to hear the case count climb by the minute as we worked quickly to adjust our policies and enact our most restrictive safety measures since the start of the pandemic.
Our protocols focused on a series of stepwise measures to reduce high-risk interactions and potential opportunities for transmission. This included pausing access to indoor facilities such as the libraries, gym and residence common areas, reinforcing our masking/face covering policy (which at the time included an outdoor masking mandate in our town), shifting from indoor dining to grab-and-go meals, and as a last resort, in-room quarantine and a shift to all remote classes, allowing students to leave their rooms only for meal pickup and outdoor solo exercise. Each of these decisions triggered a series of downstream challenges. For example, grab-and-go dining meant a change in what foods could be prepared and packaged into to-go boxes, which severely limited meal options. We also quickly had to reorganize our custodial staff to manage the overflow of waste generated from hundreds of students per dorm disposing of packaging from their three meals each day. These unintended consequences from each policy change required immediate simultaneous planning and problem solving.
Isolation and quarantine needs
In addition to supporting the students who were still healthy, our student health services team had to stretch to cover the needs of the growing number of students in both isolation and quarantine. At the peak of this outbreak, we had 143 active student cases, and through our contact investigations, we identified and were managing over 300 close contacts. Many of our students living off-campus were able to isolate or quarantine in their homes, but if not, we offered them a room in our on-campus spaces reserved for these purposes. Once diagnosed with COVID-19, on-campus students were moved from their dorm room (and a shared bathroom situation) into a residence dedicated to isolation. Meanwhile, their close contacts were moved into single rooms in one of our quarantine residences. Managing student relocations was a major undertaking. Safe transportation needed to be arranged (if this involved more than a comfortable walking distance, the use of a specially outfitted vehicle and a driver in full protective personal equipment were required). Our student affairs team monitored bed census and availability continuously to be able to immediately assign a room to the next exposed or infected student, and with input from student health services, tracked each students’ expected release from isolation or quarantine.
It was also critical to do daily check-ins with our isolating and quarantining students. Our teams would assess daily for any medical or mental health concerns that might require a clinician visit as well as other basic practical needs such as when a student forgot to pack their toothbrush or ran out of shampoo. When students asked if they could return home to isolate or quarantine, our student health services providers worked with the students and their families to determine if safe transport in a private vehicle could be arranged. We can’t emphasize strongly enough the importance of communication to our students, their families, our campus employees and the local community. We sent regular email updates to both broad and targeted (e.g., student only) audiences, and our provost hosted a weekly livestream series of “Community Conversations” to provide additional updates and respond to questions, along with a rotation of invited COVID-19 Task Force members.
Containing the outbreak
We are pleased to report that our constant vigilance, real-time monitoring, and swift and preemptive actions successfully contained this 2021 outbreak. Cases and average PCR test positivity rates for our employee population and the local community remained stable throughout. After its peak on day 11, our daily student case count had already returned to our baseline of less than 10 by day 20 (see Figure 1). Our 7-day average PCR test positivity rate among students reached 1.5%, the highest it had ever been. As we witness the current impact of the highly transmissible Omicron variant, this rate now seems enviably low. Each new variant of concern will provide new opportunities to test our response systems, but our growing experience with outbreak management, in addition to the benefits gained from the high vaccination rates of most campus communities, bodes well for any future outbreaks we may face.
For further reading
Staff Report. Dartmouth reports 119 active cases of COVID-19. Valley News, Feb. 28, 2021.
Doyle-Burr N. Dartmouth COVID-19 case counts continue to decline. Valley News, March 8, 2021.


