IDSA 2024 Guideline Update on the Risk Assessment, Diagnostic Imaging, and Microbiological Evaluation of Complicated Intra-abdominal Infections in Adults, Children, and Pregnant People
Published by IDSA,
Published by CID, July 5, 2024 | Clinical Infectious Diseases, ciae346, https://doi.org/10.1093/cid/ciae346
Robert A. Bonomo, Anthony W. Chow, Morven S. Edwards, Romney Humphries, Pranita D. Tamma, Fredrick M. Abrahamian, Mary Bessesen, E. Patchen Dellinger, Ellie Goldstein, Mary K. Hayden, Keith Kaye, Brian Potoski, Jesús Rodríguez Baño, Robert Sawyer, Marion Skalweit, David R. Snydman, Sarah Pahlke, Katelyn Donnelly, Jennifer Loveless
An overview manuscript can be found here.
Update History
This is Part 1 of an update to the 2010 SIS/IDSA Guidelines on Diagnosing and Managing Complicated Intra-Abdominal Infections in Adults and Children.
Background
As the first part of an update to the clinical practice guideline on the diagnosis and management of complicated intra-abdominal infections in adults, children, and pregnant people, developed by the Infectious Diseases Society of America, we present 21 updated recommendations. These recommendations span risk assessment, diagnostic imaging, and microbiological evaluation. The panel’s recommendations are based upon evidence derived from systematic literature reviews and adhere to a standardized methodology for rating the certainty of evidence and strength of recommendation according to the GRADE (Grading of Recommendations Assessment, Development, and Evaluation) approach.
A complicated intra-abdominal infection (cIAI) extends beyond the hollow viscus of origin into the peritoneal space or an otherwise sterile region of the abdominal cavity and is associated with peritonitis with or without abscess formation. This terminology is not meant to describe the infection’s severity or anatomy. An uncomplicated intra-abdominal infection involves only intramural inflammation of the gastrointestinal tract without extension into the peritoneal space and can progress to a complicated infection if not adequately treated.
Methods
The panel included clinicians with expertise in infectious diseases, pediatric infectious diseases, surgery, emergency medicine, microbiology, and pharmacology. Selected reviewers included clinicians with expertise in radiology, infectious diseases, and microbiology. The following organizations reviewed and provided feedback on the associated manuscripts: American Society for Microbiology, European Society of Clinical Microbiology and Infectious Diseases, Pediatric Infectious Diseases Society.
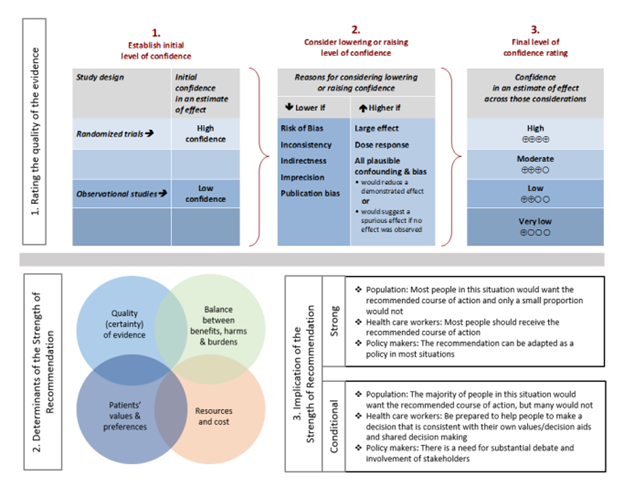
For each question, a systematic review was performed to identify relevant studies, and the GRADE (Grading of Recommendations Assessment, Development and Evaluation) approach was followed for assessing the certainty of evidence and strength of recommendation (Figure 1).
Details of the systematic review and guideline development processes are available in the supplemental materials for each included manuscript.
Figure 1. Approach and implications to rating the quality of evidence and strength of recommendations using GRADE methodology (unrestricted use of figure granted by the U.S. GRADE Network)
Recommendation: Severity of Illness Scoring Tools
This recommendation is endorsed by the European Society of Clinical Microbiology and Infectious Diseases (ESCMID) and the Pediatric Infectious Diseases Society (PIDS)
Section last reviewed and updated 06/13/2024
Last literature search conducted 10/22/2022
[View supplemental material here]
In adults and children with complicated intra-abdominal infection, which severity of illness score for risk stratification calculated within 24 hours of hospital or intensive care unit (ICU) admission best predicts 30-day or in-hospital mortality?
Recommendation
Risk stratification according to severity of illness is important for management of complicated intra-abdominal infection. For adults with complicated intra-abdominal infection, if a severity of illness score is used, the panel suggests APACHE II (Acute Physiology Age Chronic Health Evaluation II) as the preferred severity of illness score for risk stratification within 24 hours of hospital or ICU admission (conditional* recommendation, low certainty of evidence).
Remarks
• Because the WSES (World Society of Emergency Surgery) Sepsis Severity Score is specific to complicated intra-abdominal infection and performs well, it is an acceptable alternative to APACHE II for adults with complicated intra-abdominal infection.
• No severity of illness scoring system specific to complicated intra-abdominal infection can be recommended to guide management of pediatric patients with complicated intra-abdominal infection at present.
*Conditional recommendations are made when the suggested course of action would apply to the majority of people with many exceptions, and shared decision-making is important.
Results
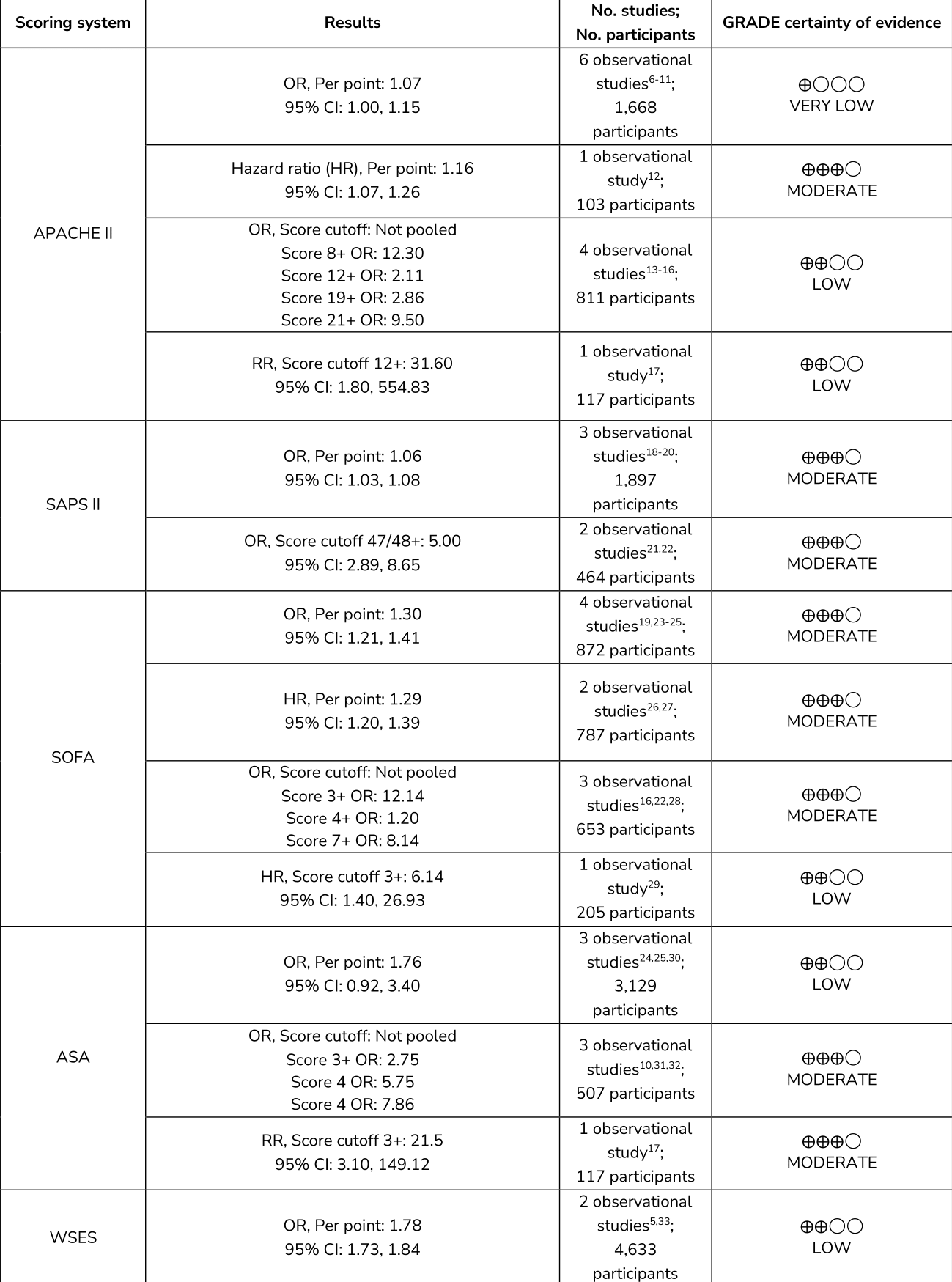
Over 20 different severity of illness scoring systems have been reported in the studies found. The four most common scoring systems were all disease-nonspecific and included: APACHE II,1 SOFA (Sequential Organ Failure Assessment),2 SAPS II (Simplified Acute Physiology Score II),3 and ASA (American Society of Anesthesiologists).4 These four scoring systems were selected for systematic review and meta-analyses. The WSES Sepsis Severity score5 for patients with complicated intra-abdominal infection was also analyzed.
Scoring Systems as Predictors for Mortality in Adults
Rationale for Recommendations
APACHE II was chosen over other severity of illness scoring systems for risk assessment of patients with complicated intra-abdominal infection because: a) even though this tool is disease-non-specific, it has been rigorously tested in patients with complicated intra-abdominal infection and variable severity of illness; b) it appears to be valid independent of the source or site of infection; c) it has acceptable discriminative power as determined by ROC assessment; d) in a retrospective study of 544 patients with complicated intra-abdominal infection, after multivariate analysis of 37 variables, it was found to be one of six independent predictors for mortality, whereas SOFA was not34; e) it is relatively easy to calculate for all patients within 24 hours of hospital admission, and a user-friendly calculator is available online (http://www.globalrph.com/apacheii.htm).
SOFA was not selected for three reasons: a) SOFA was developed originally to sequentially assess the degree of multiple organ failure in critically ill patients with sepsis, but is not suitable for categorizing patients with low-moderate severity without sepsis or organ failure within 24 hours of hospital admission; b) SOFA was not intended to indicate the success or failure of interventions or to influence medical management2; c) SOFA assesses the dysfunction of six organ systems (respiratory, cardiovascular, neurologic, renal, hepatic, coagulation) but does not take into consideration age and chronic health or comorbidities, which are important components of APACHE II. Although SAPS II performed well, it was evaluated in five studies with more limited study populations. Additionally, only one study reported ROC data for discriminative power. Similarly, ASA was evaluated in seven studies and was found to be an independent predictor for mortality in only four. ASA is also less precise and subject to inter-observer bias compared to other severity scoring systems.35 WSES Sepsis Severity Score, the only disease-specific scoring tool for complicated intra-abdominal infection, also performed well; however, only moderately ill patients were included in these studies. This scoring system was developed and validated based on findings of a large multicenter study of complicated intra-abdominal infection patients spanning 54 countries worldwide,5 and then validated in two single-center prospective studies from the United Arab Emirates (multivariate model)33 and Kenya (univariate model).36 Importantly, the overall mortality in these studies was relatively low, ranging from 1% to 12.8% (mean 9.1%), and the most common complicated intra-abdominal infection included in these studies were perforated appendicitis or duodenal perforation. It is unclear if the WSES sepsis severity score is generalizable to more seriously ill patients.
At present, no specific risk stratification scheme can be recommended to guide management of pediatric patients with complicated intra-abdominal infection. Although some scoring systems, including PRISM (Pediatric Risk of Mortality),37 PIM (Pediatric Index of Mortality),38 and PELOD-2 (Pediatric Logistic Organ Dysfunction-2)39 have been validated for children admitted to pediatric intensive care units (PICUs), they are primarily used as tools for quality assessment and performance measures of PICUs. Their utility as a tool to guide individual patient management in disease-specific conditions such as complicated intra-abdominal infection both inside and outside of the PICU setting remains unclear.
References
1. Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med 1985; 13(10): 818-29.
2. Vincent JL, Moreno R, Takala J, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med 1996; 22(7): 707-710.
3. Le Gall JR, Lemeshow S, Saulnier F. A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA 1993; 270(24): 2957-2963.
4. Knuf KM, Maani CV, Cummings AK. Clinical agreement in the American Society of Anesthesiologists physical status classification. Perioper Med (Lond) 2018; 7:14.
5. Sartelli M, Abu-Zidan FM, Catena F, et al. Global validation of the WSES Sepsis Severity Score for patients with complicated intra-abdominal infections: a prospective multicentre study (WISS Study). World J Emerg Surg 2015; 10: 61.
6. Karvellas CJ, Dong V, Abraldes JG, Lester EL, Kumar A. The impact of delayed source control and antimicrobial therapy in 196 patients with cholecystitis-associated septic shock: a cohort analysis. Can J Surg 2019; 62(3): 189-198.
7. Lichtenstern C, Herold C, Mieth M, et al. Relevance of Candida and other mycoses for morbidity and mortality in severe sepsis and septic shock due to peritonitis. Mycoses 2015; 58(7): 399-407.
8. Pan J, Zhu Q, Zhang X, et al. Factors influencing the prognosis of patients with intra-abdominal infection and its value in assessing prognosis. Infect Drug Resist 2021; 14: 3425-3432.
9. Politano AD, Hranjec T, Rosenberger LH, Sawyer RG, Tache Leon CA. Differences in morbidity and mortality with percutaneous versus open surgical drainage of postoperative intra-abdominal infections: a review of 686 cases. Am Surg 2011; 77(7): 862-867.
10. Tartaglia D, Marin JN, Nicoli AM, et al. Predictive factors of mortality in open abdomen for abdominal sepsis: a retrospective cohort study on 113 patients. Updates Surg 2021; 73(5): 1975-1982.
11. Tellor B, Skrupky LP, Symons W, High E, Micek ST, Mazuski JE. Inadequate source control and inappropriate antibiotics are key determinants of mortality in patients with intra-abdominal sepsis and associated bacteremia. Surg Infect (Larchmt) 2015; 16(6): 785-793.
12. Ozdogan HK, Karateke F, Ozyazici S, et al. The predictive value of red cell distribution width levels on mortality in intensive care patients with community-acquired intra-abdominal sepsis. Ulus Travma Acil Cerrahi Derg 2015; 21(5): 352-357.
13. Guilbart M, Zogheib E, Ntouba A, et al. Compliance with an empirical antimicrobial protocol improves the outcome of complicated intra-abdominal infections: a prospective observational study. Br J Anaesth 2016; 117(1): 66-72.
14. Li WS, Lee CH, Liu JW. Antifungal therapy did not improve outcomes including 30-day all-cause mortality in patients suffering community-acquired perforated peptic ulcer-associated peritonitis with Candida species isolated from their peritoneal fluid. J Microbiol Immunol Infect 2017; 50(3): 370-376.
15. Morais M, Goncalves D, Bessa-Melo R, Devesa V, Costa-Maia J. The open abdomen: analysis of risk factors for mortality and delayed fascial closure in 101 patients. Porto Biomed J 2018; 3(2): e14.
16. Wu Q, Ren J, Wang G, et al. The incidence, clinical outcomes, and risk factors of thrombocytopenia in intra-abdominal infection patients: A retrospective cohort study. PLoS One 2016; 11(1): e0147482.
17. Buck DL, Vester-Andersen M, Moller MH. Accuracy of clinical prediction rules in peptic ulcer perforation: An observational study. Scand J Gastroenterol 2012; 47(1): 28-35.
18. De Waele J, Lipman J, Sakr Y, et al. Abdominal infections in the intensive care unit: characteristics, treatment and determinants of outcome. BMC Infect Dis 2014; 14: 420.
19. Dupont H, Friggeri A, Touzeau J, et al. Enterococci increase the morbidity and mortality associated with severe intra-abdominal infections in elderly patients hospitalized in the intensive care unit. J Antimicrob Chemother 2011; 66(10): 2379-2385.
20. Maseda E, Ramirez S, Picatto P, et al. Critically ill patients with community-onset intraabdominal infections: Influence of healthcare exposure on resistance rates and mortality. PLoS One 2019; 14(9): e0223092.
21. Alqarni A, Kantor E, Grall N, et al. Clinical characteristics and prognosis of bacteraemia during postoperative intra-abdominal infections. Crit Care 2018; 22(1): 175.
22. Suarez-de-la-Rica A, Maseda E, Anillo V, et al. Biomarkers (procalcitonin, C reactive protein, and lactate) as predictors of mortality in surgical patients with complicated intra-abdominal infection. Surgical Infections 2015; 16(3): 346-351.
23. Augustin P, Tanaka S, Tran-Dinh A, et al. Outcome and adequacy of empirical antibiotherapy in post-operative peritonitis: A retrospective study. Surg Infect (Larchmt) 2020; 21(3): 284-292.
24. Pupelis G, Drozdova N, Mukans M, Malbrain ML. Serum procalcitonin is a sensitive marker for septic shock and mortality in secondary peritonitis. Anestezjol 2014; 46(4): 262-273.
25. Sim J, Hong SS, Kwak JY, Jung YT. Prediction of culture-positive sepsis and selection of empiric antibiotics in critically ill patients with complicated intra-abdominal infections: a retrospective study. Eur J Trauma Emerg Surg 2020; 48(2): 963-971.
26. Luo X, Li L, Ou S, Zeng Z, Chen Z. Risk factors for mortality in abdominal infection patients in ICU: A retrospective study from 2011 to 2018. Front Med (Lausanne) 2022; 9: 839284.
27. Montravers P, Augustin P, Grall N, et al. Characteristics and outcomes of anti-infective de-escalation during health care-associated intra-abdominal infections. Crit Care 2016; 20: 83.
28. Nugraha GL, Danardono E. A retrospective study of factors affecting mortality in patients with complicated intra-abdominal infection. Med J Malaysia 2022; 77(5): 612-618.
29. Roger C, Garrigue D, Bouhours G, et al. Time to source control and outcome in community-acquired intra-abdominal infections: The multicentre observational PERICOM study. Eur J Anaesthesiol 2022; 39: 540-548.
30. Moller MH, Engebjerg MC, Adamsen S, et al. The Peptic Ulcer Perforation (PULP) score: a predictor of mortality following peptic ulcer perforation. A cohort study. Acta Anaesthesiol Scan 2012; 56: 655-662.
31. Bensignor T, Lefevre JH, Creavin B, et al. Postoperative peritonitis after digestive tract surgery: Surgical management and risk factors for morbidity and mortality, a cohort of 191 patients. World J Surg 2018; 42: 3589-3598.
32. Faes S, Hubner M, Girardin T, Demartines N, Hahnloser D. Rate of stoma formation following damage-control surgery for severe intra-abdominal sepsis: a single-centre consecutive case series. BJS Open 2021; 5(6).
33. Abdel-Kader S, Sartelli M, Abu-Zidan FM. Complicated intra-abdominal infections: a prospective validation study of the WSES Sepsis Severity Score. Singapore Med J 2019; 60(6): 317-321.
34. Huang S, Chen L, Liu J, et al. Novel multiparametric nomogram for overall survival prediction in complicated intra-abdominal infection: A multicenter study in China. Front Med (Lausanne) 2021; 8: 627416.
35. Blamey SL, Imrie CW, O'Neill J, Gilmour WH, Carter DC. Prognostic factors in acute pancreatitis. Gut 1984; 25(12): 1340-1346.
36. Mwenda KI, Daniel O, Mark A. Utility of World Society of Emergency Surgery Sepsis Severity Score in predicting outcomes of intra-abdominal infections. Ann Afr Surg 2020; 17: 65-68.
37. Costa GA, Delgado AF, Ferraro A, Okay TS. Application of the pediatric risk of mortality (PRISM) score and determination of mortality risk factors in a tertiary pediatric intensive care unit. Clinics (Sao Paulo) 2010; 65(11): 1087-1092.
38. Shann F, Pearson G, Slater A, Wilkinson K. Paediatric index of mortality (PIM): a mortality prediction model for children in intensive care. Intensive Care Med 1997; 23(2): 201-207.
39. Leteurtre S, Duhamel A, Salleron J et al. PELOD-2: An update of the PEdiatric Logistic Organ Dysfunction Score. Crit Care Med. 2013; 41(7): 1761-1773.
Recommendation: Diagnostic Imaging for Suspected Acute Appendicitis (Adults)
This recommendation is endorsed by the European Society of Clinical Microbiology and Infectious Diseases (ESCMID)
Section last reviewed and updated 06/13/2024
Last literature search conducted 10/22/2022
[View supplemental material here]
In adults with suspected acute appendicitis, should ultrasound (US), CT, or MRI be obtained as the initial imaging modality?
In adults with suspected appendicitis, if initial imaging is inconclusive, should US, CT, or MRI be obtained for subsequent imaging?
Recommendation
In non-pregnant adults with suspected acute appendicitis, the panel suggests obtaining an abdominal CT as the initial imaging modality to diagnose acute appendicitis (conditional* recommendation, very low certainty of evidence).
Remarks
• IV contrast is usually appropriate whenever a CT is obtained in adults with suspected acute appendicitis; however, CT without IV contrast also has high diagnostic accuracy in detecting acute appendicitis and may be appropriate.1
• Because of CT’s accuracy, immediate additional imaging studies beyond CT are usually not necessary. If a CT is negative but clinical suspicion for acute appendicitis persists, consider observation and supportive care, with or without antibiotics; if clinical suspicion is high, consider surgical intervention.
• US, when definitively positive or definitively negative, and MRI are also reasonably accurate and may precede CT, depending on the patient and clinical circumstances.
*Conditional recommendations are made when the suggested course of action would apply to the majority of people with many exceptions, and shared decision-making is important.
Results
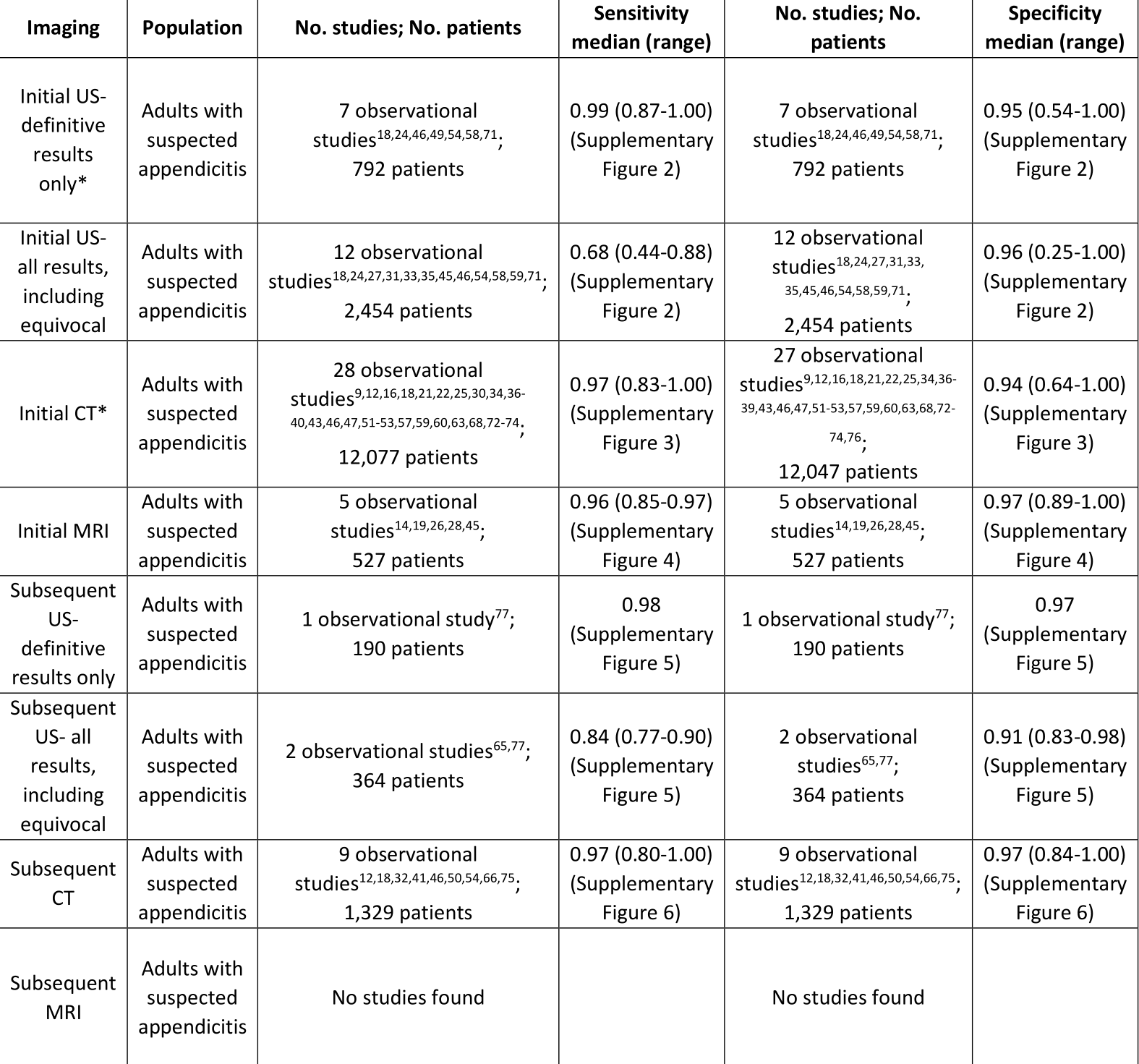
A comprehensive search and review of five selected meta-analyses2-6 yielded a total of 69 primary observational studies7-75 for the analyses on whether to use CT, US, or MRI to diagnose acute appendicitis in adults.
Summary of Evidence for Imaging Modalities Compared to Pathology for Diagnosing Acute Appendicitis in Adults
*One additional study78 performed a head-to-head comparison of US and CT in adults presenting to the ED with abdominal pain. For the 284 diagnosed with appendicitis, US (definitive results only) and CT yielded sensitivities of 76% and 94%, respectively, and specificities of 95% and 95%, respectively.
Rationale for Recommendations
Abdominal CT is suggested as the initial imaging modality for adults with suspected acute appendicitis. Although US seems highly accurate when yielding definitive results, abdominal CT can be used to identify other potential causes of abdominal pain (e.g., colon cancer) that are more likely to be seen in adults. Because of this, the panel suggests CT as the initial imaging modality for adults. Because of CT’s accuracy in diagnosing acute appendicitis, additional imaging studies beyond CT should not be necessary. US, when definitively positive or definitively negative, and MRI are also reasonably accurate and may precede CT, depending on the patient and clinical circumstances.
References
1. Expert Panel on Gastrointestinal I, Kambadakone AR, Santillan CS, et al. ACR appropriateness criteria(R) right lower quadrant pain: 2022 update. J Am Coll Radiol 2022; 19(11S): S445-S461.
2. D'Souza N, Hicks G, Beable R, Higginson A, Rud B. Magnetic resonance imaging (MRI) for diagnosis of acute appendicitis. Cochrane Database Syst Rev 2021; 12(12): CD012028.
3. Eng KA, Abadeh A, Ligocki C, et al. Acute appendicitis: a meta-analysis of the diagnostic accuracy of US, CT, and MRI as second-line imaging tests after an initial US. Radiology 2018; 288(3): 717-727.
4. Arruzza E, Milanese S, Li LSK, Dizon J. Diagnostic accuracy of computed tomography and ultrasound for the diagnosis of acute appendicitis: A systematic review and meta-analysis. Radiography (Lond) 2022; 28(4): 1127-1141.
5. Rud B, Vejborg TS, Rappeport ED, Reitsma JB, Wille-Jorgensen P. Computed tomography for diagnosis of acute appendicitis in adults. Cochrane Database Syst Rev 2019; 2019(11).
6. Dahabreh IJ, Adam GP, Halladay CW, et al. Diagnosis of right lower auadrant pain and suspected acute appendicitis. Rockville (MD), 2015.
7. Alnuaymah F, Etonyeaku AC, Alsaeed HS, et al. Clinical, radiological and pathological appraisal of acute appendicitis in Al Qassim, Saudi Arabia: a single-center retrospective analysis. Cureus 2022; 14(8): e28627.
8. Alshebromi MH, Alsaigh SH, Aldhubayb MA. Sensitivity and specificity of computed tomography and ultrasound for the prediction of acute appendicitis at King Fahad Specialist Hospital in Buraidah, Saudi Arabia. Saudi Med J 2019; 40(5): 458-462.
9. Apisarnthanarak P, Suvannarerg V, Pattaranutaporn P, Charoensak A, Raman SS, Apisarnthanarak A. Alvarado score: can it reduce unnecessary CT scans for evaluation of acute appendicitis? Am J Emerg Med 2015; 33(2): 266-270.
10. Aras A, Karaman E, Peksen C, Kiziltan R, Kotan MC. The diagnosis of acute appendicitis in pregnant versus non-pregnant women: A comparative study. Rev Assoc Med Bras (1992) 2016; 62(7): 622-627.
11. Ashcroft J, Singh AA, Rooney S, Bennett J, Davies RJ. A single centre evaluation of risk prediction models and imaging modalities in acute appendicitis. Ann R Coll Surg Engl 2021; 103(3): 203-207.
12. Atema JJ, Gans SL, Van Randen A, et al. Comparison of imaging strategies with conditional versus Immediate contrast-enhanced computed tomography in patients with clinical suspicion of acute appendicitis. Eur Radiol 2015; 25(8): 2445-2452.
13. Atwood R, Blair S, Fisk M, Bradley M, Coleman C, Rodriguez C. NSQIP based predictors of false negative and indeterminate ultrasounds in adults with appendicitis. J Surg Res 2021; 261: 326-333.
14. Avcu S, Cetin FA, Arslan H, Kemik O, Dulger AC. The value of diffusion-weighted imaging and apparent diffusion coefficient quantification in the diagnosis of perforated and nonperforated appendicitis. Diagn Interv Radiol 2013; 19(2): 106-110.
15. Chabanova E, Balslev I, Achiam M, et al. Unenhanced MR imaging in adults with clinically suspected acute appendicitis. Eur J Radiol 2011; 79(2): 206-210.
16. Chu LL, Webb EM, Stengel JW, Yeh BM, Lu Y, Coakley FV. CT of acute appendicitis: can diagnostic accuracy serve as a practical performance metric for readers specialized in abdominal imaging? Clin Imaging 2014; 38(1): 56-59.
17. Coursey CA, Nelson RC, Moreno RD, Patel MB, Beam CA, Vaslef S. Appendicitis, body mass index, and CT: is CT more valuable for obese patients than thin patients? Am Surg 2011; 77(4): 471-475.
18. Crocker C, Akl M, Abdolell M, Kamali M, Costa AF. Ultrasound and CT in the diagnosis of appendicitis: accuracy with consideration of indeterminate examinations according to STARD Guidelines. AJR Am J Roentgenol 2020; 215(3): 639-644.
19. Ziedses des Plantes CMP, van Veen MJF, van der Palen J, Klaase JM, Gielkens HAJ, Geelkerken RH. The effect of unenhanced MRI on the surgeons' decision-making process in females with suspected appendicitis. World J Surg 2016; 40(12): 2881-2887.
20. Donlon NE, Kelly ME, Sheppard A, et al. Negative appendicectomy rates as a quality measure in a regional surgical unit: a retrospective review. Ir J Med Sci 2021; 190(2): 755-761.
21. Dowhanik A, Tonkopi E, Crocker CE, Costa AF. Diagnostic performance and radiation dose of reduced vs. standard scan range abdominopelvic CT for evaluation of appendicitis. Eur Radiol 2021; 31(10): 7817-7826.
22. Eurboonyanun K, Rungwiriyawanich P, Chamadol N, Promsorn J, Eurboonyanun C, Srimunta P. Accuracy of nonenhanced CT vs contrast-enhanced CT for diagnosis of acute appendicitis in adults. Curr Probl Diagn Radiol 2021; 50(3): 315-320.
23. Fatima SR, Zaheer F, Moosa FA, Arqam SM, Mussab RM, Choudhry MS. Combined diagnostic accuracy of total leukocyte count, neutrophil count, and ultrasonography for the diagnosis of acute appendicitis. Cureus 2021; 13(2): e13086.
24. Fedko M, Bellamkonda VR, Bellolio MF, et al. Ultrasound evaluation of appendicitis: importance of the 3 x 2 table for outcome reporting. Am J Emerg Med 2014; 32(4): 346-348.
25. Hekimoglu K, Yildirim UM, Karabulut E, Coskun M. Comparison of combined oral and i.v. contrast-enhanced versus single i.v. contrast-enhanced mdct for the detection of acute appendicitis. JBR-BTR 2011; 94(5): 278-282.
26. Heverhagen JT, Pfestroff K, Heverhagen AE, Klose KJ, Kessler K, Sitter H. Diagnostic accuracy of magnetic resonance imaging: a prospective evaluation of patients with suspected appendicitis (diamond). J Magn Reson Imaging 2012; 35(3): 617-623.
27. Hussain S, Rahman A, Abbasi T, Aziz T. Diagnostic accuracy of ultrasonography in acute appendicitis. J Ayub Med Coll Abbottabad 2014; 26(1): 12-17.
28. Inci E, Hocaoglu E, Aydin S, et al. Efficiency of unenhanced MRI in the diagnosis of acute appendicitis: comparison with Alvarado scoring system and histopathological results. Eur J Radiol 2011; 80(2): 253-258.
29. Jakkula J. A clinical study and ultrasonography diagnosis in clinically suspected cases of acute appendicitis. European Journal of Molecular & Clinical Medicine 2022; 9(4): 1-11.
30. Jo YH, Kim K, Rhee JE, et al. The accuracy of emergency medicine and surgical residents in the diagnosis of acute appendicitis. Am J Emerg Med 2010; 28(7): 766-770.
31. John SK, Joseph J, Shetty SR. Avoiding negative appendectomies in rural surgical practice: is C-reactive protein estimation useful as a diagnostic tool? Natl Med J India 2011; 24(3): 144-147.
32. Jones RP, Jeffrey RB, Shah BR, Desser TS, Rosenberg J, Olcott EW. Journal club: the Alvarado score as a method for reducing the number of CT studies when appendiceal ultrasound fails to visualize the appendix in adults. AJR Am J Roentgenol 2015; 204(3): 519-526.
33. Kapoor A, Kapoor A, Mahajan G. Real-time elastography in acute appendicitis. J Ultrasound Med 2010; 29(6): 871-877.
34. Karabulut N, Kiroglu Y, Herek D, Kocak TB, Erdur B. Feasibility of low-dose unenhanced multi-detector CT in patients with suspected acute appendicitis: comparison with sonography. Clin Imaging 2014; 38(3): 296-301.
35. Karimi E, Aminianfar M, Zarafshani K, Safaie A. The accuracy of emergency physicians in ultrasonographic screening of acute appendicitis; a cross sectional study. Emerg (Tehran) 2017; 5(1): e22.
36. Kepner AM, Bacasnot JV, Stahlman BA. Intravenous contrast alone vs intravenous and oral contrast computed tomography for the diagnosis of appendicitis in adult ED patients. Am J Emerg Med 2012; 30(9): 1765-1773.
37. Kim K, Kim YH, Kim SY, et al. Low-dose abdominal CT for evaluating suspected appendicitis. N Engl J Med 2012; 366(17): 1596-1605.
38. Kim SY, Lee KH, Kim K, et al. Acute appendicitis in young adults: low- versus standard-radiation-dose contrast-enhanced abdominal CT for diagnosis. Radiology 2011; 260(2): 437-445.
39. Ko Y, Lee WJ, Park JH, et al. Diagnostic sensitivity and specificity of 2-mSv CT vs. conventional-dose CT in adolescents and young adults with suspected appendicitis: post hoc subgroup analysis of the LOCAT data. Eur Radiol 2020; 30(8): 4573-4585.
40. Kolb M, Storz C, Kim JH, et al. Effect of a novel denoising technique on image quality and diagnostic accuracy in low-dose CT in patients with suspected appendicitis. Eur J Radiol 2019; 116: 198-204.
41. Koo HS, Kim HC, Yang DM, Kim SW, Park SJ, Ryu JK. Does computed tomography have any additional value after sonography in patients with suspected acute appendicitis? J Ultrasound Med 2013; 32(8): 1397-1403.
42. Kouame N, N'Goan-Domoua AM, N'Dri K J, et al. The diagnostic value of indirect ultrasound signs during acute adult appendicitis. Diagn Interv Imaging 2012; 93(3): e24-e28.
43. Latifi A, Labruto F, Kaiser S, Ullberg U, Sundin A, Torkzad MR. Does enteral contrast increase the accuracy of appendicitis diagnosis? Radiol Technol 2011; 82(4): 294-299.
44. Leeuwenburgh MM, Wiarda BM, Wiezer MJ, et al. Comparison of imaging strategies with conditional contrast-enhanced CT and unenhanced MR imaging in patients suspected of having appendicitis: a multicenter diagnostic performance study. Radiology 2013; 268(1): 135-143.
45. Leeuwenburgh MM, Wiezer MJ, Wiarda BM, et al. Accuracy of MRI compared with ultrasound imaging and selective use of CT to discriminate simple from perforated appendicitis. Br J Surg 2014; 101(1): e147-e155.
46. Leung YK, Chan CP, Graham CA, Rainer TH. Acute appendicitis in adults: diagnostic accuracy of emergency doctors in a university hospital in Hong Kong. Emerg Med Australas 2017; 29(1): 48-55.
47. Lietzen E, Salminen P, Rinta-Kiikka I, et al. The accuracy of the computed tomography diagnosis of acute appendicitis: does the experience of the radiologist matter? Scand J Surg 2018; 107(1): 43-47.
48. Liu W, Wei Qiang J, Xun Sun R. Comparison of multislice computed tomography and clinical scores for diagnosing acute appendicitis. J Int Med Res 2015; 43(3): 341-349.
49. Luksaite-Lukste R, Kliokyte R, Samuilis A, et al. Conditional CT strategy-an effective tool to reduce negative appendectomy rate and the overuse of the CT. J Clin Med 2021; 10(11): 2456.
50. O'Malley ME, Alharbi F, Chawla TP, Moshonov H. CT following US for possible appendicitis: anatomic coverage. Eur Radiol 2016; 26(2): 532-538.
51. Öztürk A, Bozkurtoğlu H, Üçkurt Y, Kaya C, Yananlı ZD, Akıncı ÖF. The effect of computed tomography on surgeon’s decisions in suspected appendicitis cases Şüpheli Apandisit Olgularında Bilgisayarlı Tomografinin Cerrahın Kararları Üzerine Etkisi. J Clin Anal Med 2015; 6(6): 716-719.
52. Park JH, Kim B, Kim MS, et al. Comparison of filtered back projection and iterative reconstruction in diagnosing appendicitis at 2-mSv CT. Abdom Radiol (NY) 2016; 41(7): 1227-1236.
53. Pickhardt PJ, Lawrence EM, Pooler BD, Bruce RJ. Diagnostic performance of multidetector computed tomography for suspected acute appendicitis. Ann Intern Med 2011; 154(12): 789-796, W-291.
54. Poletti PA, Platon A, De Perrot T, et al. Acute appendicitis: prospective evaluation of a diagnostic algorithm integrating ultrasound and low-dose CT to reduce the need of standard CT. Eur Radiol 2011; 21(12): 2558-2566.
55. Rait JS, Ajzajian J, McGillicuddy J, Sharma A, Andrews B. Acute appendicitis and the role of pre-operative imaging: A cohort study. Ann Med Surg (Lond) 2020; 59: 258-263.
56. Reich B, Zalut T, Weiner SG. An international evaluation of ultrasound vs. computed tomography in the diagnosis of appendicitis. Int J Emerg Med 2011; 4: 68.
57. Repplinger MD, Pickhardt PJ, Robbins JB, et al. Prospective comparison of the diagnostic accuracy of MR imaging versus CT for acute appendicitis. Radiology 2018; 288(2): 467-475.
58. Roberts JM, van de Poll T, Hague CJ, Murray N. Ultrasound for suspected acute appendicitis in adult women under age 40: an evaluation of on-call radiology resident scanning. Acad Radiol 2021; 28(8): 1169-1173.
59. Sammalkorpi HE, Leppaniemi A, Lantto E, Mentula P. Performance of imaging studies in patients with suspected appendicitis after stratification with adult appendicitis score. World J Emerg Surg 2017; 12: 6.
60. Scott AJ, Mason SE, Arunakirinathan M, Reissis Y, Kinross JM, Smith JJ. Risk stratification by the appendicitis inflammatory response score to guide decision-making in patients with suspected appendicitis. Br J Surg 2015; 102(5): 563-572.
61. Gebre Selassie H, Tekle Selassie H, Ashebir D. Pattern and outcome of acute appendicitis: observational prospective study from a teaching hospital, Addis Ababa, Ethiopia. Open Access Emerg Med 2021; 13: 265-271.
62. Serinsoz S, Akturk R. Can diffusion-weighted imaging be a gold standard method for acute appendicitis? A comparative study. I J Radiol 2021; 18(3): e113603.
63. Sim JY, Kim HJ, Yeon JW, et al. Added value of ultrasound re-evaluation for patients with equivocal CT findings of acute appendicitis: a preliminary study. Eur Radiol 2013; 23(7): 1882-1890.
64. Singh R SB. Combined diagnostic value of Modified Alvarado Score (MAS) and ultrasound for the diagnosis of acute appendicitis. International Journal of Pharmaceutical and Clinical Research 2022; 14(9): 28-33.
65. Sohail S, Siddiqui KJ. Doptaus--a simple criterion for improving sonographic diagnosis of acute appendicitis. J Pak Med Assoc 2009; 59(2): 79-82.
66. Stabile Ianora AA, Moschetta M, Lorusso V, Scardapane A. Atypical appendicitis: diagnostic value of volume-rendered reconstructions obtained with 16-slice multidetector-row CT. Radiol Med 2010; 115(1): 93-104.
67. Sukhani PK, Gumber N, Vyas C. The diagnosis of acute appendicitis by ultrasonography in pregnant and non-pregnant women: a comparative study. Int J Med Sci Educ 2017; 4(3): 210-215.
68. Tan WJ, Acharyya S, Goh YC, et al. Prospective comparison of the Alvarado score and CT scan in the evaluation of suspected appendicitis: a proposed algorithm to guide CT use. J Am Coll Surg 2015; 220(2): 218-224.
69. Tatli F, Ekici U, Kanlioz M, et al. Ultrasonography in diagnosis of acute appendicitis. Ann Ital Chir 2016; 87: 152-154.
70. Teo AT, Lefter LP, Zarrouk AJ, Merrett ND. Institutional review of patients presenting with suspected appendicitis. ANZ J Surg 2015; 85(6): 420-424.
71. Tyler PD, Carey J, Stashko E, Levenson RB, Shapiro NI, Rosen CL. The potential role of ultrasound in the work-up of appendicitis in the emergency department. J Emerg Med 2019; 56(2): 191-196.
72. Uzunosmanoglu H, Cevik Y, Corbacioglu SK, Akinci E, Bulus H, Agladioglu K. Diagnostic value of appendicular Doppler ultrasonography in acute appendicitis. Ulus Travma Acil Cerrahi Derg 2017; 23(3): 188-192.
73. Wagner PJ, Haroon M, Morarasu S, Eguare E, Al-Sahaf O. Does CT reduce the rate of negative laparoscopies for acute appendicitis? A single-center retrospective study. J Med Life 2020; 13(1): 26-31.
74. Wang SY, Fang JF, Liao CH, et al. Prospective study of computed tomography in patients with suspected acute appendicitis and low Alvarado score. Am J Emerg Med 2012; 30(8): 1597-1601.
75. Wongwaisayawan S TP, Klawandee S, Prapruttam D. . Diagnostic performance and reliability of the standardized computed tomography reporting system for acute appendicitis: experience in a tertiary care academic center. J Med Assoc Thai 2021; 104(7): 1102-1108.
76. Aguilera F, Gilchrist BF, Farkas DT. Accuracy of MRI in diagnosing appendicitis during pregnancy. Am Surg 2018; 84(8): 1326-1328.
77. Gungor F, Kilic T, Akyol KC, et al. Diagnostic value and effect of bedside ultrasound in acute appendicitis in the emergency department. Acad Emerg Med 2017; 24(5): 578-586.
78. van Randen A, Lameris W, van Es HW, et al. A comparison of the accuracy of ultrasound and computed tomography in common diagnoses causing acute abdominal pain. Eur Radiol 2011; 21(7): 1535-1545.
Recommendation: Diagnostic Imaging for Suspected Acute Appendicitis (Children)
This recommendation is endorsed by the European Society of Clinical Microbiology and Infectious Diseases (ESCMID) and the Pediatric Infectious Diseases Society (PIDS)
Section last reviewed and updated 06/13/2024
Last literature search conducted 10/22/2022
[View supplemental material here]
In children with suspected acute appendicitis, should ultrasound (US), CT, or MRI be obtained as the initial imaging modality?
Recommendation
In children and adolescents with suspected acute appendicitis, the panel suggests obtaining an abdominal US as the initial imaging modality to diagnose acute appendicitis (conditional* recommendation, very low certainty of evidence).
Remarks
• US is generally readily available but is also operator-dependent and can yield equivocal results. MRI is not always readily available, and sedation may be required for young children. CT is generally readily available but involves radiation exposure and may require use of IV contrast or sedation.
*Conditional recommendations are made when the suggested course of action would apply to the majority of people with many exceptions, and shared decision-making is important.
In children with suspected appendicitis, if initial imaging is inconclusive, should US, CT, or MRI be obtained for subsequent imaging?
Recommendation
In children and adolescents with suspected acute appendicitis, if initial US is equivocal/non-diagnostic and clinical suspicion persists, the panel suggests obtaining an abdominal MRI or CT as subsequent imaging to diagnose acute appendicitis rather than obtaining another US (conditional* recommendation, very low certainty of evidence).
Remarks
• US is generally available but is also operator-dependent and can yield equivocal results. MRI is not always readily available, and sedation may be required for young children. CT is generally readily available but involves radiation exposure and may require use of IV contrast or sedation.
• CT with IV contrast is usually appropriate when performed in children with suspected acute appendicitis after equivocal ultrasound; however, CT without IV contrast may be appropriate.1
• Depending on the clinical situation, observation may be appropriate instead of subsequent imaging.
• If there is a strong clinical suspicion for appendicitis after equivocal imaging, exploratory laparoscopy or laparotomy may also be considered if subsequent imaging delays appropriate management.
*Conditional recommendations are made when the suggested course of action would apply to the majority of people with many exceptions, and shared decision-making is important.
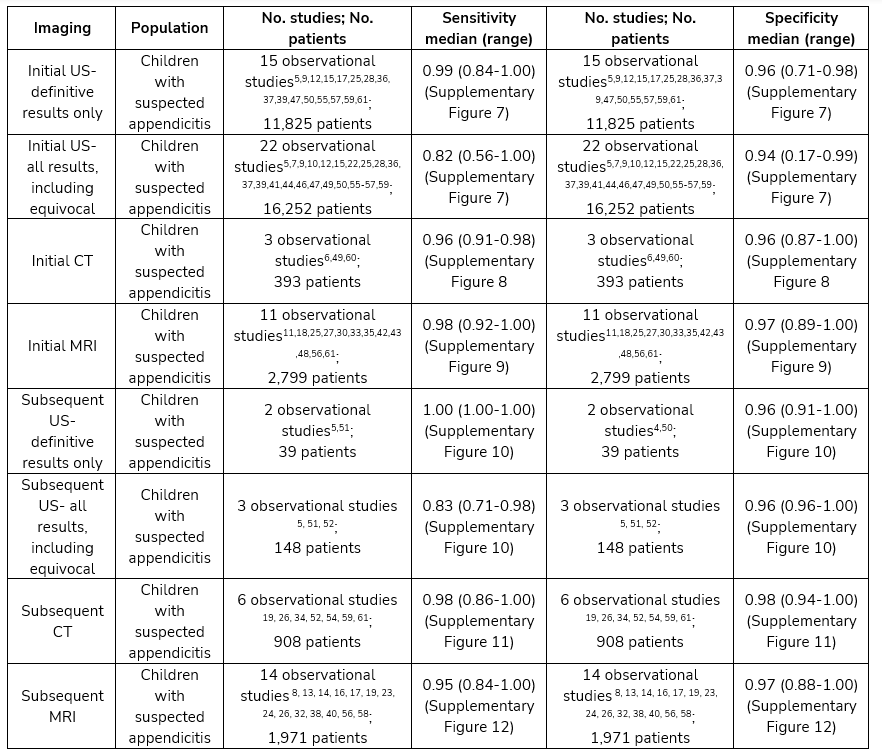
Results
A comprehensive search and review of three selected meta-analyses [2-4] yielded 56 primary observational studies [5-60] for the analyses on whether to use CT, US, or MRI to diagnose acute appendicitis in children.
Summary of Evidence for Imaging Modalities Compared to Pathology for Diagnosing Acute Appendicitis in Children
Rationale for Recommendations
The panel suggests US as the preferred initial imaging modality in children with suspected acute appendicitis. If an initial US is equivocal/indeterminate, the panel suggests either MRI or CT for subsequent imaging. Both CT and MRI demonstrated very high sensitivities and specificities. US had comparable results when considering only definitively positive and definitively negative imaging interpretations. When adding in the equivocal/indeterminate results, sensitivity of US dropped from 99% to 82%. Because US is readily available, inexpensive, and highly accurate when yielding a definitive result, the panel suggests obtaining an US first in children with suspected appendicitis. MRI may not be as readily available and may necessitate sedation in young children. CT is associated with radiation exposure, which is of particular concern in children. However, US often yields equivocal/indeterminate results, in which case, the panel suggests either MRI or CT as subsequent imaging in children with suspected appendicitis. Allergies or contraindications to IV contrast may preclude the use of CT.
References
1. Expert Panel on Pediatric I, Koberlein GC, Trout AT, et al. ACR appropriateness criteria® suspected appendicitis-child. J Am Coll Radiol 2019; 16(5S): S252-S263.
2. D'Souza N, Hicks G, Beable R, Higginson A, Rud B. Magnetic resonance imaging (MRI) for diagnosis of acute appendicitis. Cochrane Database Syst Rev 2021; 12(12): CD012028.
3. Eng KA, Abadeh A, Ligocki C, et al. Acute appendicitis: a meta-analysis of the diagnostic accuracy of US, CT, and MRI as second-line imaging tests after an initial US. Radiology 2018; 288(3): 717-727.
4. Zhang H, Liao M, Chen J, Zhu D, Byanju S. Ultrasound, computed tomography or magnetic resonance imaging - which is preferred for acute appendicitis in children? A meta-analysis. Pediatr Radiol 2017; 47(2): 186-196.
5. Ahmad T, Khdair Ahmad F, Manson D. Diagnostic performance of a staged pathway for imaging acute appendicitis in children. Pediatr Emerg Care 2021; 37(12): e1197-e1201.
6. Akhtar W, Ali S, Arshad M, Ali FN, Nadeem N. Focused abdominal CT scan for acute appendicitis in children: can it help in need? J Pak Med Assoc 2011; 61(5): 474-476.
7. Ashjaei B, Mehdizadeh M, Alizadeh H, Najm N, Moghtaderi M. Evaluating the value of different sonographic findings in diagnosis of acute appendicitis in children. Afr J Paediatr Surg 2022; 19(1): 13-17.
8. Aspelund G, Fingeret A, Gross E, et al. Ultrasonography/MRI versus CT for diagnosing appendicitis. Pediatrics 2014; 133(4): 586-593.
9. Austin-Page LR, Pham PK, Elkhunovich M. Evaluating changes in diagnostic accuracy of ultrasound for appendicitis: does practice make perfect? J Emerg Med 2020; 59(4): 563-72.
10. Aydin D, Turan C, Yurtseven A, et al. Integration of radiology and clinical score in pediatric appendicitis. Pediatr Int 2018; 60(2): 173-178.
11. Bayraktutan U, Oral A, Kantarci M, et al. Diagnostic performance of diffusion-weighted MR imaging in detecting acute appendicitis in children: comparison with conventional MRI and surgical findings. J Magn Reson Imaging 2014; 39(6): 1518-1524.
12. Binkovitz LA, Unsdorfer KM, Thapa P, et al. Pediatric appendiceal ultrasound: accuracy, determinacy and clinical outcomes. Pediatr Radiol 2015; 45(13): 1934-1944.
13. Corkum KS, Oyetunji TA, Grabowski JE, Rigsby CK, Lautz TB. Absolute neutrophil count as a diagnostic guide for the use of MRI in the workup of suspected appendicitis in children. J Pediatr Surg 2019; 54(7): 1359-1364.
14. Covelli JD, Madireddi SP, May LA, Costello JE, Lisanti CJ, Carlson CL. MRI for pediatric appendicitis in an adult-focused general hospital: a clinical effectiveness study-challenges and lessons learned. AJR Am J Roentgenol 2019; 212(1): 180-187.
15. Cundy TP, Gent R, Frauenfelder C, Lukic L, Linke RJ, Goh DW. Benchmarking the value of ultrasound for acute appendicitis in children. J Pediatr Surg 2016; 51(12): 1939-1943.
16. Davis J, Chima M, Kasmire K. Radiation-free diagnosis of pediatric appendicitis: accuracy of point-of-care ultrasonography and magnetic resonance imaging. Pediatr Emerg Care 2022; 38(1): e246-e250.
17. Dibble EH, Swenson DW, Cartagena C, Baird GL, Herliczek TW. Effectiveness of a staged US and unenhanced MR imaging algorithm in the diagnosis of pediatric appendicitis. Radiology 2018; 286(3): 1022-1029.
18. Didier RA, Hopkins KL, Coakley FV, Krishnaswami S, Spiro DM, Foster BR. Performance characteristics of magnetic resonance imaging without contrast agents or sedation in pediatric appendicitis. Pediatr Radiol 2017; 47(10): 1312-1320.
19. Dillman JR, Gadepalli S, Sroufe NS, et al. Equivocal pediatric appendicitis: unenhanced MR imaging protocol for nonsedated children-a clinical effectiveness study. Radiology 2016; 279(1): 216-225.
20. Ferrarese A, Falcone A, Solej M, et al. Surgeon's clinical valuation and accuracy of ultrasound in the diagnosis of acute appendicitis: A comparison with intraoperative evaluation. Five years experience. Int J Surg 2016; 33 Suppl 1: S45-50.
21. Gungor F, Kilic T, Akyol KC, et al. Diagnostic value and effect of bedside ultrasound in acute appendicitis in the emergency department. Acad Emerg Med 2017; 24(5): 578-586.
22. Harel S, Mallon M, Langston J, Blutstein R, Kassutto Z, Gaughan J. Factors contributing to nonvisualization of the appendix on ultrasound in children with suspected appendicitis. Pediatr Emerg Care 2022; 38(2): e678-e682.
23. Herliczek TW, Swenson DW, Mayo-Smith WW. Utility of MRI after inconclusive ultrasound in pediatric patients with suspected appendicitis: retrospective review of 60 consecutive patients. AJR Am J Roentgenol 2013; 200(5): 969-973.
24. Heye P, Saavedra JSM, Victoria T, Laje P. Accuracy of unenhanced, non-sedated MRI in the diagnosis of acute appendicitis in children. J Pediatr Surg 2020; 55(2): 253-256.
25. Imler D, Keller C, Sivasankar S, et al. Magnetic resonance imaging versus ultrasound as the initial imaging modality for pediatric and young adult patients with suspected appendicitis. Acad Emerg Med 2017; 24(5): 569-577.
26. James NC, Ahmadian R, McKee JQ, et al. Magnetic resonance imaging availability reduces computed tomography use for pediatric appendicitis diagnosis. Pediatr Emerg Care 2022; 38(1): e219-e224.
27. Johnson AK, Filippi CG, Andrews T, et al. Ultrafast 3-T MRI in the evaluation of children with acute lower abdominal pain for the detection of appendicitis. AJR Am J Roentgenol 2012; 198(6): 1424-1430.
28. Kearl YL, Claudius I, Behar S, et al. Accuracy of magnetic resonance imaging and ultrasound for appendicitis in diagnostic and nondiagnostic studies. Acad Emerg Med 2016; 23(2): 179-185.
29. Kelly BS, Bollard SM, Weir A, et al. Improving diagnostic accuracy in clinically ambiguous paediatric appendicitis: a retrospective review of ultrasound and pathology findings with focus on the non-visualised appendix. Br J Radiol 2019; 92(1093): 20180585.
30. Kennedy TM, Thompson AD, Choudhary AK, Caplan RJ, Schenker KE, DePiero AD. Utility of applying white blood cell cutoffs to non-diagnostic MRI and ultrasound studies for suspected pediatric appendicitis. Am J Emerg Med 2019; 37(9): 1723-1728.
31. Koc C, Akbulut S, Coskun EI, Sarici B, Yilmaz S. Comparison of the demographic and clinical features of pregnant and non-pregnant patients undergoing appendectomy. Ulus Travma Acil Cerrahi Derg 2020; 26(4): 555-562.
32. Komanchuk J, Martin DA, Killam R, et al. Magnetic resonance imaging provides useful diagnostic information following equivocal ultrasound in children with suspected appendicitis. Can Assoc Radiol J 2021; 72(4): 797-805.
33. Koning JL, Naheedy JH, Kruk PG. Diagnostic performance of contrast-enhanced MR for acute appendicitis and alternative causes of abdominal pain in children. Pediatr Radiol 2014; 44(8): 948-955.
34. Krishnamoorthi R, Ramarajan N, Wang NE, et al. Effectiveness of a staged US and CT protocol for the diagnosis of pediatric appendicitis: reducing radiation exposure in the age of ALARA. Radiology 2011; 259(1): 231-239.
35. Kulaylat AN, Moore MM, Engbrecht BW, et al. An implemented MRI program to eliminate radiation from the evaluation of pediatric appendicitis. J Pediatr Surg 2015; 50(8): 1359-63.
36. Limchareon S, Wongsuttilert A, Boonyarit A. Efficacy of ultrasonography in the evaluation of suspected appendicitis in a pediatric population. Journal of Medical Ultrasound 2014; 22(4): 213-217.
37. Lofvenberg F, Salo M. Ultrasound for appendicitis: performance and integration with clinical parameters. Biomed Res Int 2016; 2016: 5697692.
38. Lyons GR, Renjen P, Askin G, Giambrone AE, Beneck D, Kovanlikaya A. Diagnostic utility of intravenous contrast for MR imaging in pediatric appendicitis. Pediatr Radiol 2017; 47(4): 398-403.
39. Mangona KLM, Guillerman RP, Mangona VS, et al. Diagnostic performance of ultrasonography for pediatric appendicitis: a night and day difference? Acad Radiol 2017; 24(12): 1616-1620.
40. Martin JF, Mathison DJ, Mullan PC, Otero HJ. Secondary imaging for suspected appendicitis after equivocal ultrasound: time to disposition of MRI compared to CT. Emerg Radiol 2018; 25(2): 161-168.
41. Mirza WA, Naveed MZ, Khandwala K. Utility and accuracy of primary and secondary ultrasonographic signs for diagnosing acute appendicitis in pediatric patients. Cureus 2018; 10(12): e3779.
42. Moore MM, Gustas CN, Choudhary AK, et al. MRI for clinically suspected pediatric appendicitis: an implemented program. Pediatr Radiol 2012; 42(9): 1056-1063.
43. Mushtaq R, Desoky SM, Morello F, et al. First-line diagnostic evaluation with MRI of children suspected of having acute appendicitis. Radiology 2019; 291(1): 170-177.
44. Nandan R, Samie AU, Acharya SK, et al. Pediatric appendicitis score or ultrasonography? In search of a better diagnostic tool in Indian children with lower abdominal pain. Indian J Pediatr 2023; 90(12): 1204-1209.
45. Pedram A, Asadian F, Roshan N. Diagnostic accuracy of abdominal ultrasonography in pediatric acute appendicitis. Bull Emerg Trauma 2019; 7(3): 278-283.
46. Salim J, Agustina F, Maker JJR. Pre-Coronavirus disease 2019 pediatric acute appendicitis: risk factors model and diagnosis modality in a developing low-income country. Pediatr Gastroenterol Hepatol Nutr 2022; 25(1): 30-40.
47. Salman R, Sher AC, Guillerman RP, et al. Acute appendicitis and SARS-CoV-2 in children: imaging findings at a tertiary children's hospital during the COVID-19 pandemic. Pediatr Radiol 2022; 52(3): 460-467.
48. Sawyer DM, Mushtaq R, Vedantham S, et al. Performance of overnight on-call radiology residents in interpreting unenhanced abdominopelvic magnetic resonance imaging studies performed for pediatric right lower quadrant abdominal pain. Pediatr Radiol 2021; 51(8): 1378-1385.
49. Sayed AO, Zeidan NS, Fahmy DM, Ibrahim HA. Diagnostic reliability of pediatric appendicitis score, ultrasound and low-dose computed tomography scan in children with suspected acute appendicitis. Ther Clin Risk Manag 2017; 13: 847-854.
50. Scammell S, Lansdale N, Sprigg A, Campbell D, Marven S. Ultrasonography aids decision-making in children with abdominal pain. Ann R Coll Surg Engl 2011; 93(5): 405-409.
51. Schuh S, Chan K, Langer JC, et al. Properties of serial ultrasound clinical diagnostic pathway in suspected appendicitis and related computed tomography use. Acad Emerg Med 2015; 22(4): 406-414.
52. Schuh S, Man C, Cheng A, et al. Predictors of non-diagnostic ultrasound scanning in children with suspected appendicitis. J Pediatr 2011; 158(1): 112-118.
53. Sezer TO, Gulece B, Zalluhoglu N, Gorgun M, Dogan S. Diagnostic value of ultrasonography in appendicitis. Adv Clin Exp Med 2012; 21(5): 633-636.
54. Srinivasan A, Servaes S, Pena A, Darge K. Utility of CT after sonography for suspected appendicitis in children: integration of a clinical scoring system with a staged imaging protocol. Emerg Radiol 2015; 22(1): 31-42.
55. Tantisook T, Aravapalli S, Chotai PN, et al. Determining the impact of body mass index on ultrasound accuracy for diagnosing appendicitis: Is it less useful in obese children? J Pediatr Surg 2021; 56(11): 2010-2015.
56. Thieme ME, Leeuwenburgh MM, Valdehueza ZD, et al. Diagnostic accuracy and patient acceptance of MRI in children with suspected appendicitis. Eur Radiol 2014; 24(3): 630-637.
57. Toprak H, Kilincaslan H, Ahmad IC, et al. Integration of ultrasound findings with Alvarado score in children with suspected appendicitis. Pediatr Int 2014; 56(1): 95-99.
58. Tung EL, Baird GL, Ayyala RS, Sams C, Herliczek TW, Swenson DW. Comparison of MRI appendix biometrics in children with and without acute appendicitis. Eur Radiol 2022; 32(2): 1024-1033.
59. van Atta AJ, Baskin HJ, Maves CK, et al. Implementing an ultrasound-based protocol for diagnosing appendicitis while maintaining diagnostic accuracy. Pediatr Radiol 2015; 45(5): 678-685.
60. Didier RA. Iterative reconstruction technique with reduced volume CT dose index: Diagnostic accuracy in pediatric acute appendicitis. Pediatr Radiol 2015; 45(2): 181-187.
61. Aguilera F, Gilchrist BF, Farkas DT. Accuracy of MRI in diagnosing appendicitis during pregnancy. Am Surg 2018; 84(8): 1326-1328.
Recommendation: Diagnostic Imaging for Suspected Acute Appendicitis (Pregnant People)
This recommendation is endorsed by the European Society of Clinical Microbiology and Infectious Diseases (ESCMID)
Section last reviewed 06/13/2024
Last literature search conducted 10/22/2022
[View supplemental material here]
In pregnant people with suspected acute appendicitis, should ultrasound (US) or MRI be obtained as the initial imaging modality?
Recommendation
In pregnant people with suspected acute appendicitis, the panel suggests obtaining an abdominal US as the initial imaging modality to diagnose acute appendicitis (conditional* recommendation, very low certainty of evidence).
Remarks
• It would also be reasonable to initially obtain an MRI in pregnant people with suspected acute appendicitis if access to an MRI is readily available. The conditional imaging strategy suggested (US, then MRI for equivocal results) would likely yield the same results as an MRI only.
*Conditional recommendations are made when the suggested course of action would apply to the majority of people with many exceptions, and shared decision-making is important.
In pregnant people with suspected appendicitis, if initial imaging is inconclusive, should US or MRI be obtained for subsequent imaging?
Recommendation
In pregnant people with suspected acute appendicitis, if initial US is equivocal/non-diagnostic and clinical suspicion persists, the panel suggests obtaining an MRI as subsequent imaging to diagnose acute appendicitis (conditional* recommendation, very low certainty evidence).
Remarks
• It would also be reasonable to initially obtain an MRI in pregnant people with suspected acute appendicitis if access to an MRI is readily available. The conditional imaging strategy suggested (US, then MRI for equivocal results) would likely yield the same results as an MRI only.
*Conditional recommendations are made when the suggested course of action would apply to the majority of people with many exceptions, and shared decision-making is important.
Results
A comprehensive search and review of five selected meta-analyses1-5 yielded 26 primary observational studies6-31 for the analyses on whether to use CT, US, or MRI to diagnose acute appendicitis in pregnant people.
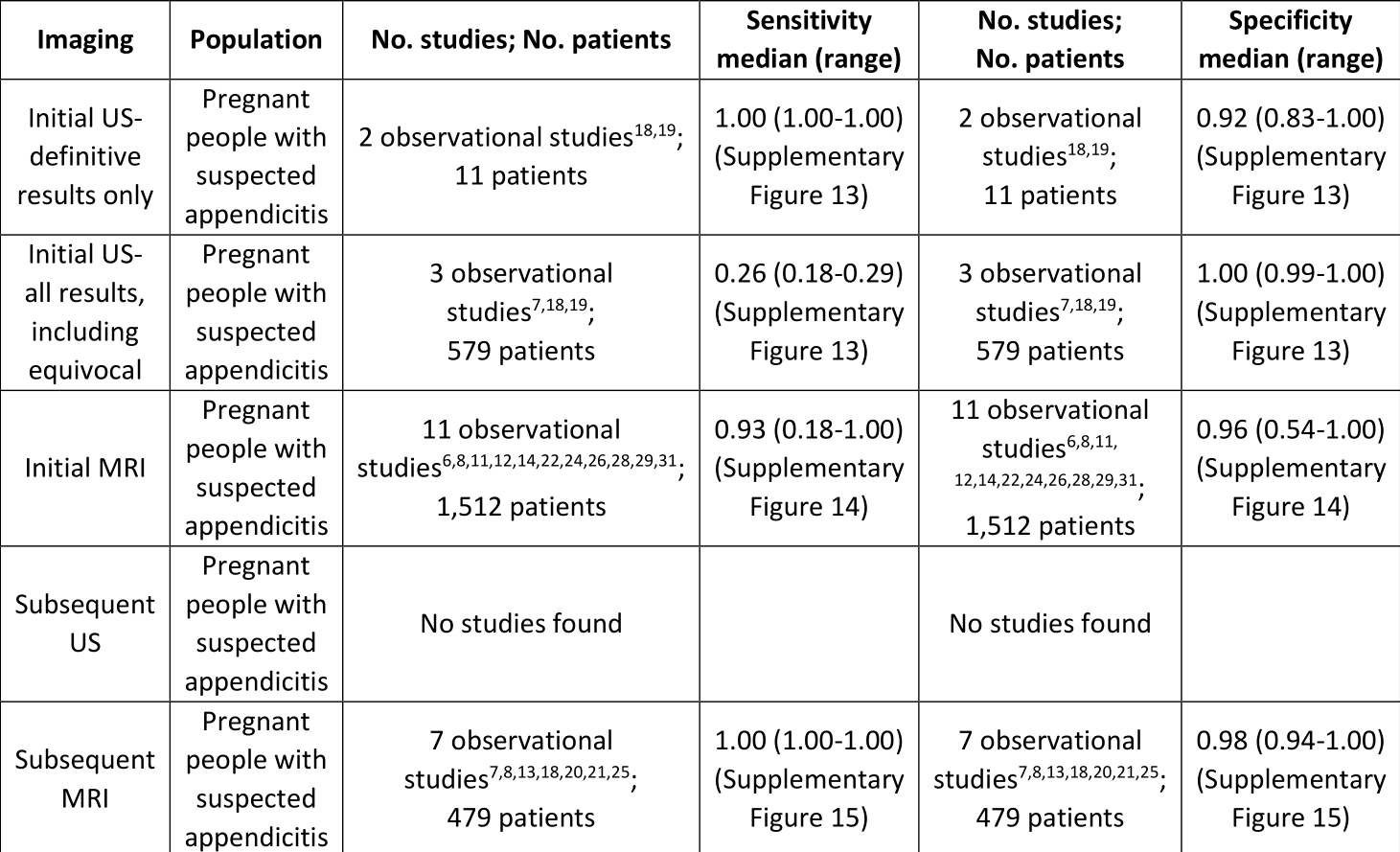
Summary of Evidence for Imaging Modalities Compared to Pathology for Diagnosing Acute Appendicitis in Pregnant People
Rationale for Recommendations
Abdominal US is suggested as the initial imaging modality for pregnant people with suspected acute appendicitis. If the initial US is equivocal, the panel suggests obtaining an MRI as subsequent imaging to diagnose acute appendicitis. While limited by an extremely small sample size (n=11), combined data suggest that initial US results are accurate when definitive results are reported. For most pregnant people reporting pain congruent with suspected acute appendicitis, practitioners would likely perform an initial US as part of the assessment because of the ease of access to an US. MRI following an initial US is also highly accurate and is suggested for subsequent imaging beyond US. It would also be reasonable for a practitioner to proceed directly to an MRI as the initial imaging modality, if available and feasible.
References
1. D'Souza N, Hicks G, Beable R, Higginson A, Rud B. Magnetic resonance imaging (MRI) for diagnosis of acute appendicitis. Cochrane Database Syst Rev 2021; 12(12): CD012028.
2. Dahabreh IJ, Adam GP, Halladay CW, et al. Diagnosis of right lower auadrant pain and suspected acute appendicitis. Rockville (MD), 2015.
3. Eng KA, Abadeh A, Ligocki C, et al. Acute appendicitis: a meta-analysis of the diagnostic accuracy of US, CT, and MRI as second-line imaging tests after an initial US. Radiology 2018; 288(3): 717-727.
4. Moghadam MN, Salarzaei M, Shahraki Z. Diagnostic accuracy of ultrasound in diagnosing acute appendicitis in pregnancy: a systematic review and meta-analysis. Emerg Radiol 2022; 29(3): 437-448.
5. Li Y, Li S. Potential of ultrasound in the evaluation of acute appendicitis during pregnancy: a systematic review and meta-analysis. CEOG 2022; 49(1).
6. Aguilera F, Gilchrist BF, Farkas DT. Accuracy of MRI in diagnosing appendicitis during pregnancy. Am Surg 2018; 84(8): 1326-1328.
7. Ahmed B, Williams J, Gourash W, et al. MRI as first line imaging for suspected acute appendicitis during pregnancy: diagnostic accuracy and level of inter-radiologist agreement. Curr Probl Diagn Radiol 2022; 51(4): 503-510.
8. Amitai MM, Katorza E, Guranda L, et al. Role of emergency magnetic resonance imaging for the workup of suspected appendicitis in pregnant women. Isr Med Assoc J 2016; 18(10): 600-604.
9. Aras A, Karaman E, Peksen C, Kiziltan R, Kotan MC. The diagnosis of acute appendicitis in pregnant versus non-pregnant women: A comparative study. Rev Assoc Med Bras (1992) 2016; 62(7): 622-627.
10. Baruch Y, Canetti M, Blecher Y, Yogev Y, Grisaru D, Michaan N. The diagnostic accuracy of ultrasound in the diagnosis of acute appendicitis in pregnancy. J Matern Fetal Neonatal Med 2020; 33(23): 3929-3934.
11. Burke LM, Bashir MR, Miller FH, et al. Magnetic resonance imaging of acute appendicitis in pregnancy: a 5-year multiinstitutional study. Am J Obstet Gynecol 2015; 213(5): 693.e1-6.
12. Donlon NE, Kelly ME, Sheppard A, et al. Negative appendicectomy rates as a quality measure in a regional surgical unit: a retrospective review. Ir J Med Sci 2021; 190(2): 755-761.
13. Fonseca AL, Schuster KM, Kaplan LJ, Maung AA, Lui FY, Davis KA. The use of magnetic resonance imaging in the diagnosis of suspected appendicitis in pregnancy: shortened length of stay without increase in hospital charges. JAMA Surgery 2014; 149(7): 687-693.
14. Jang KM, Kim SH, Choi D, Lee SJ, Rhim H, Park MJ. The value of 3D T1-weighted gradient-echo MR imaging for evaluation of the appendix during pregnancy: preliminary results. Acta Radiol 2011; 52(8): 825-828.
15. Kapan M, Onder A, Tekbas G, et al. Percutaneous cholecystostomy in high-risk elderly patients with acute cholecystitis: a lifesaving option. Am J Hosp Palliat Care 2013; 30(2): 167-171.
16. Kazemini A, Reza Keramati M, Fazeli MS, Keshvari A, Khaki S, Rahnemai-Azar A. Accuracy of ultrasonography in diagnosing acute appendicitis during pregnancy based on surgical findings. Med J Islam Repub Iran 2017; 31: 48.
17. Koc C, Akbulut S, Coskun EI, Sarici B, Yilmaz S. Comparison of the demographic and clinical features of pregnant and non-pregnant patients undergoing appendectomy. Ulus Travma Acil Cerrahi Derg 2020; 26(4): 555-562.
18. Konrad J, Grand D, Lourenco A. MRI: first-line imaging modality for pregnant patients with suspected appendicitis. Abdom Imaging 2015; 40(8): 3359-3364.
19. Lehnert BE, Gross JA, Linnau KF, Moshiri M. Utility of ultrasound for evaluating the appendix during the second and third trimester of pregnancy. Emerg Radiol 2012; 19(4): 293-299.
20. Lukenaite B, Luksaite-Lukste R, Mikalauskas S, Samuilis A, Strupas K, Poskus T. Magnetic resonance imaging reduces the rate of unnecessary operations in pregnant patients with suspected acute appendicitis: a retrospective study. Ann Surg Treat Res 2021; 100(1): 40-46.
21. Masselli G, Brunelli R, Casciani E, et al. Acute abdominal and pelvic pain in pregnancy: MR imaging as a valuable adjunct to ultrasound? Abdom Imaging 2011; 36(5): 596-603.
22. Meesa IR, Mammen L. MR imaging of pregnant women with abdominal pain and suspected appendicitis: diagnostic accuracy and outcomes. International Journal of Radiology and Radiation Oncology 2011; 2: 4-7.
23. Mejri A, Arfaoui K, Trigui E. Acute appendicitis in pregnant women: A Tunisian center experience. Medicine (Baltimore) 2022; 101(29): e28574.
24. Patel D, Fingard J, Winters S, Low G. Clinical use of MRI for the evaluation of acute appendicitis during pregnancy. Abdom Radiol (NY) 2017; 42(7): 1857-1863.
25. Ramalingam V, LeBedis C, Kelly JR, Uyeda J, Soto JA, Anderson SW. Evaluation of a sequential multi-modality imaging algorithm for the diagnosis of acute appendicitis in the pregnant female. Emerg Radiol 2015; 22(2): 125-132.
26. Shin I, An C, Lim JS, Kim MJ, Chung YE. T1 bright appendix sign to exclude acute appendicitis in pregnant women. Eur Radiol 2017; 27(8): 3310-3316.
27. Sukhani PK, Gumber N, Vyas C. The diagnosis of acute appendicitis by ultrasonography in pregnant and non-pregnant women: a comparative study. IntJMedSciEduc 2017; 4(3): 210-215.
28. Theilen LH, Mellnick VM, Longman RE, et al. Utility of magnetic resonance imaging for suspected appendicitis in pregnant women. Am J Obstet Gynecol 2015; 212(3): 345 e1-6.
29. Tsai R, Raptis C, Fowler KJ, Owen JW, Mellnick VM. MRI of suspected appendicitis during pregnancy: interradiologist agreement, indeterminate interpretation and the meaning of non-visualization of the appendix. Br J Radiol 2017; 90(1079): 20170383.
30. Unal A, Sayharman SE, Ozel L, et al. Acute abdomen in pregnancy requiring surgical management: a 20-case series. Eur J Obstet Gynecol Reprod Biol 2011; 159(1): 87-90.
31. Burns M, Hague CJ, Vos P, Tiwari P, Wiseman SM. Utility of magnetic resonance imaging for the diagnosis of appendicitis during pregnancy: a canadian experience. Can Assoc Radiol J 2017; 68(4): 392-400.
Recommendation: Diagnostic Imaging for Suspected Acute Cholecystitis or Acute Cholangitis (Adults)
This recommendation is endorsed by the European Society of Clinical Microbiology and Infectious Diseases (ESCMID) and the Pediatric Infectious Diseases Society (PIDS)
Section last reviewed and updated 06/13/2024
Last literature search conducted 10/22/2022
[View supplemental material here]
In adults with suspected acute cholecystitis or acute cholangitis, should abdominal ultrasound (US) or CT be obtained as the initial imaging modality?
Recommendation
In non-pregnant adults with suspected acute cholecystitis or acute cholangitis, the panel suggests abdominal US as the initial diagnostic imaging modality (conditional recommendation*, very low certainty of evidence).
Remarks
• The diagnosis of acute cholangitis should include clinical signs (jaundice, fever, chills, and right upper quadrant abdominal pain), laboratory findings (indicators of inflammation and biliary stasis), and imaging findings (biliary dilatation, or evidence of an etiology, e.g., stricture, stone, obstructing mass).
• We did not identify any studies assessing the accuracy of abdominal US or CT for the diagnosis of acute cholangitis and relied on indirect evidence from acute cholecystitis.
• Because acute cholecystitis and acute cholangitis are uncommon in children, we did not systematically review the evidence for children; however, it would be reasonable to mirror the imaging pathway for adults in children.
*Conditional recommendations are made when the suggested course of action would apply to the majority of people with many exceptions, and shared decision-making is important.
In adults with suspected acute cholecystitis or acute cholangitis, if initial imaging is inconclusive, should CT, MRI/MRCP (magnetic resonance cholangiopancreatography) or HIDA (hepatobiliary iminodiacetic acid) be obtained for subsequent imaging?
Recommendation
In non-pregnant adults with suspected acute cholecystitis or acute cholangitis, if initial US is equivocal/non-diagnostic and clinical suspicion persists, the panel suggests obtaining an abdominal CT scan as subsequent imaging to diagnose acute cholecystitis or acute cholangitis (conditional* recommendation, very low certainty of evidence).
Remarks
• The diagnosis of acute cholangitis should include clinical signs (jaundice, fever, chills, and right upper quadrant abdominal pain), laboratory findings (indicators of inflammation and biliary stasis), and imaging findings (biliary dilatation, or evidence of an etiology, e.g., stricture, stone, obstructing mass).
• CT with IV contrast is preferable and usually appropriate when CT is obtained for subsequent imaging.1
• We did not identify any studies assessing the accuracy of abdominal US or CT for the diagnosis of acute cholangitis and relied on indirect evidence from acute cholecystitis.
• Because acute cholecystitis and acute cholangitis are uncommon in children, we did not systematically review the evidence for children; however, it would be reasonable to mirror the imaging pathway for adults in children.
Recommendation
In non-pregnant adults with suspected acute cholecystitis, if both US and CT are equivocal/non-diagnostic and clinical suspicion persists, the panel suggests obtaining either an abdominal MRI/MRCP (magnetic resonance cholangiopancreatography) or hepatobiliary iminodiacetic acid (HIDA) scan as subsequent imaging to diagnose acute cholecystitis (conditional* recommendation, low certainty of evidence for HIDA, knowledge gap for MRI/MRCP).
Remarks
• If both abdominal US and CT are inconclusive but acute cholangitis is suspected, MRI/MRCP is a reasonable option.
• The diagnosis of acute cholangitis should include clinical signs (jaundice, fever, chills, and right upper quadrant abdominal pain), laboratory findings (indicators of inflammation and biliary stasis), and imaging findings (biliary dilatation, or evidence of an etiology, e.g., stricture, stone, obstructing mass).
• Because acute cholecystitis and acute cholangitis are uncommon in children, we did not systematically review the evidence for children; however, it would be reasonable to mirror the imaging pathway for adults in children.
*Conditional recommendations are made when the suggested course of action would apply to the majority of people with many exceptions, and shared decision-making is important.
Results
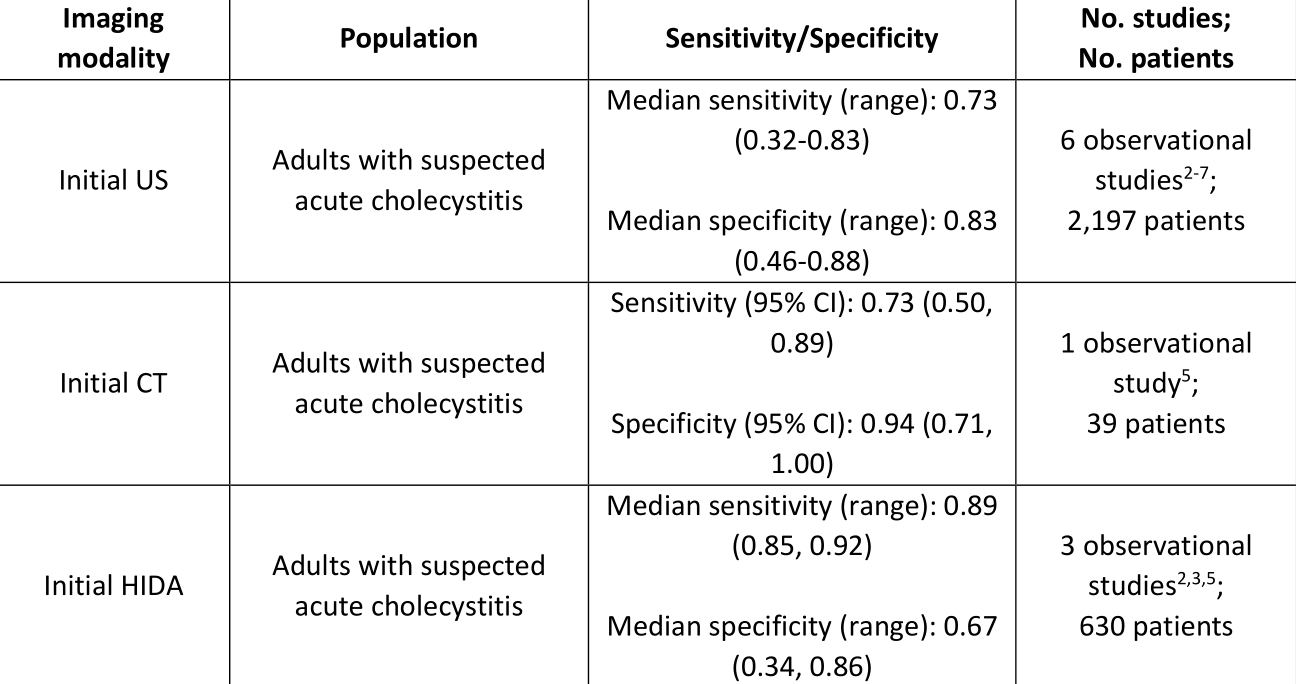
The panel identified six observational studies for the analysis on whether to use US or CT as initial imaging for diagnosing acute cholecystitis in patients with suspected acute cholecystitis.2-7 Three observational studies that reviewed the diagnostic accuracy of HIDA for suspected acute cholecystitis were identified.2,3,5 No studies addressing MRI/MRCP in patients with suspected acute cholecystitis were found, even after expanding the publication date limit by an additional five years (2005 on).
The panel did not find any studies to include in our analysis on whether to use US or CT as initial (or subsequent) imaging for diagnosing acute cholangitis. Instead, the panel considered the evidence found for acute cholecystitis as indirect evidence for this patient population. The panel thought this approach appropriate since at the time of ordering initial imaging, distinguishing between suspected cholecystitis and acute cholangitis is likely challenging.
Summary of Evidence for Imaging Modalities Compared to Pathology for Diagnosing Acute Cholecystitis
Rationale for Recommendations
In non-pregnant adults and children with suspected acute cholecystitis or acute cholangitis, US is suggested as the initial imaging modality over CT because it is reasonably accurate and useful in identifying gallstones, less costly, and more portable, and results are generally available in a timelier manner. Additional benefits include the avoidance of radiation exposure (particularly important for children) and contrast-associated side effects that may be encountered with CT. US is more operator-dependent than CT and may not be as accurate in obese patients, but the desirable effects of US outlined above outweigh these undesirable effects. CT is suggested as the subsequent imaging modality for non-pregnant adults and children due to its ability to identify complications and rule out other etiologies. If additional imaging beyond US is required, the risk-to-benefit ratio of radiation exposure for CT should be considered (particularly for children). If CT is also equivocal and acute cholecystitis, specifically, is suspected, MRI/MRCP and HIDA are both reasonable options as subsequent imaging studies beyond CT. The benefits of MRI/MRCP as compared to HIDA are that these studies provide a clearer picture of the surrounding structures and a faster time to result, in addition to being more readily available. On the other hand, HIDA is considered the gold standard for diagnosing acute cholecystitis and is far less costly than MRI/MRCP. However, a patient must fast for several hours before undergoing a HIDA scan.
Recommendation: Diagnostic Imaging for Suspected Acute Cholecystitis or Acute Cholangitis (Pregnant People)
This recommendation is endorsed by the European Society of Clinical Microbiology and Infectious Diseases (ESCMID)
[View supplemental material here]
In pregnant people with suspected acute cholecystitis or acute cholangitis, should abdominal US or MRI be obtained as the initial imaging modality?
Recommendation
In pregnant people with suspected acute cholecystitis or suspected acute cholangitis, US or MRI can be considered as the initial diagnostic imaging modality; however, the panel is unable to recommend one imaging modality versus the other (knowledge gap).
Remarks
• The diagnosis of acute cholangitis should include clinical signs (jaundice, fever, chills, and right upper quadrant abdominal pain), laboratory findings (indicators of inflammation and biliary stasis), and imaging findings (biliary dilatation, or evidence of an etiology, e.g., stricture, stone, obstructing mass).
Results
No studies addressing diagnostic accuracy of imaging modalities for pregnant patients with suspected acute cholecystitis or acute cholangitis were identified. However, the panel considered evidence from non-pregnant adults along with the balance between benefits and harms (e.g., radiation exposure) of each imaging modality.
References
1. Expert Panel on Gastrointestinal Imaging: Russo GK, Zaheer A, Kamel IR, et al. ACR Appropriateness Criteria® right upper quadrant pain: 2022 update. J Am Coll Radiol 2023; 20(5S): S211-S223.
2. Kaoutzanis C, Davies E, Leichtle SW, et al. Abdominal ultrasound versus hepato-imino diacetic acid scan in diagnosing acute cholecystitis--what is the real benefit? J Surg Res 2014; 188(1): 44-52.
3. Kaoutzanis C, Davies E, Leichtle SW, et al. Is hepato-imino diacetic acid scan a better imaging modality than abdominal ultrasound for diagnosing acute cholecystitis? Am J Surg 2015; 210(3): 473-482.
4. Naidu K, Beenen E, Gananadha S, Mosse C. The yield of fever, inflammatory markers and ultrasound in the diagnosis of acute cholecystitis: A validation of the 2013 Tokyo Guidelines. World J Surg 2016; 40(12): 2892-2897.
5. Rodriguez LE, Sanchez-Vivaldi JA, Velez-Quinones MP, et al. The impact of a rapid imaging protocol in acute cholecystitis-prospective cohort study. Int J Surg Case Rep 2018; 51: 388-394.
6. Stogryn S, Metcalfe J, Vergis A, Hardy K. Does ultrasonography predict intraoperative findings at cholecystectomy? An institutional review. Can J Surg 2016; 59(1): 12-18.
7. Summers SM, Scruggs W, Menchine MD, et al. A prospective evaluation of emergency department bedside ultrasonography for the detection of acute cholecystitis. Ann Emerg Med 2010; 56(2): 114-122.
Recommendation: Diagnostic Imaging for Suspected Acute Diverticulitis (Adults)
This recommendation is endorsed by the European Society of Clinical Microbiology and Infectious Diseases (ESCMID)
Section last reviewed and updated 06/13/2024
Last literatyre search conducted 10/22/2022
[View supplemental material here]
In adults with suspected acute diverticulitis, should CT, US (ultrasound), or MRI be obtained as the initial imaging modality?
Recommendation
In non-pregnant adults with suspected acute diverticulitis, the panel suggests obtaining an abdominal CT as the initial diagnostic modality (conditional* recommendation, very low certainty of evidence).
Remarks
• IV contrast is usually appropriate whenever a CT is obtained and can be helpful to characterize and detect subtle bowel wall abnormalities and complications of diverticulitis; however, CT without IV contrast may be appropriate.1
Recommendation
In non-pregnant adults with suspected acute diverticulitis, if CT is unavailable or contraindicated, the panel suggests obtaining an US or MRI as the initial diagnostic modality (conditional* recommendation, very low certainty of evidence).
*Conditional recommendations are made when the suggested course of action would apply to the majority of people with many exceptions, and shared decision-making is important.
Results
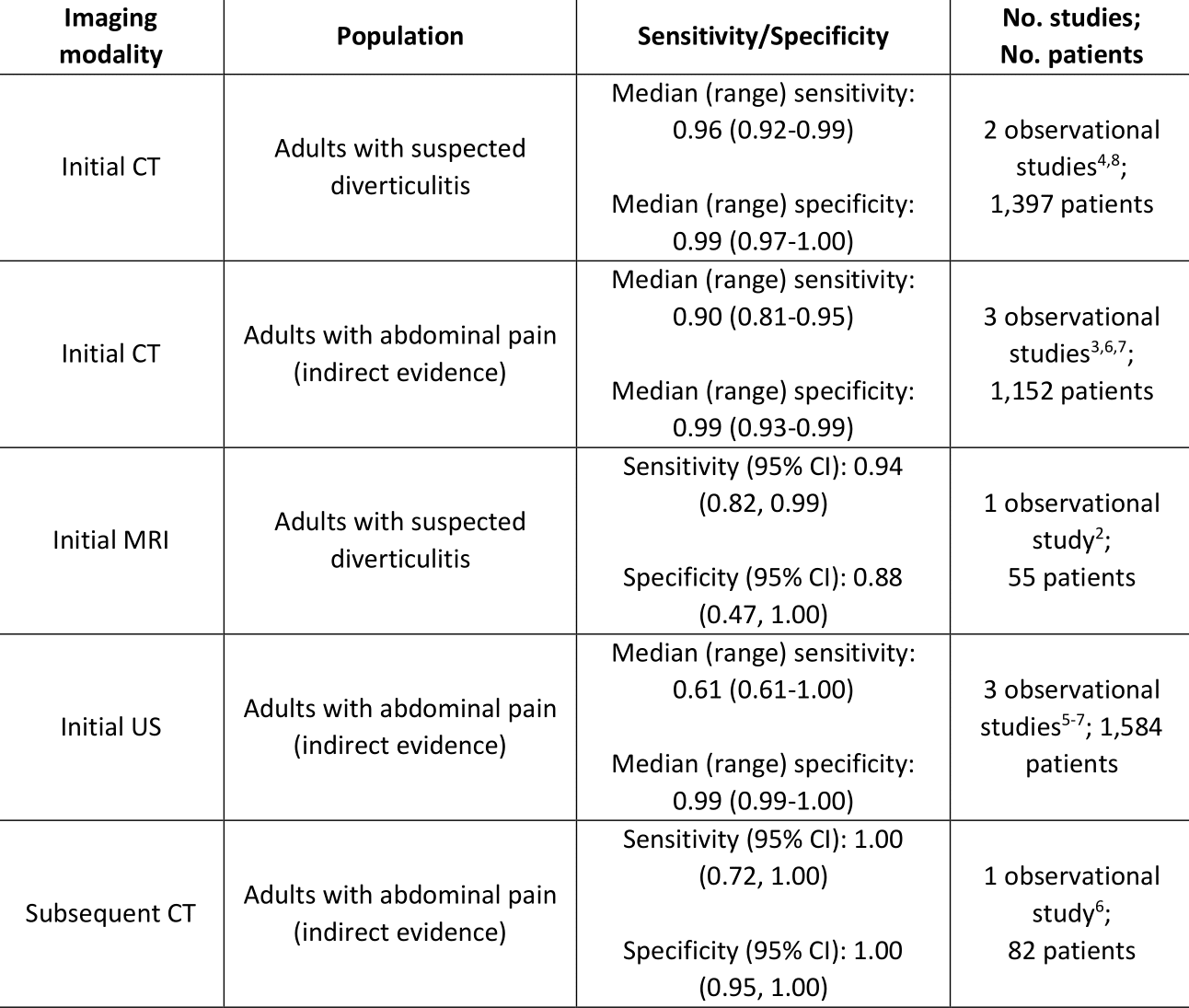
A comprehensive search identified seven observational studies meeting eligibility on whether to use CT, US, or MRI to diagnose diverticulitis.2-8 Three studies addressed the diagnostic accuracy of CT or MRI in our exact patient population, i.e., patients with suspected diverticulitis.2,4,8 The panel did not find any studies addressing the diagnostic accuracy of US in only patients with suspected diverticulitis; however, four studies addressing the diagnostic accuracy of US or CT in patients with abdominal pain were identified.3,5-7 No studies addressing the diagnostic accuracy of MRI were found for this broader patient population.
Summary of Evidence for Imaging Modalities Compared to Pathology for Diagnosing Acute Diverticulitis
Rationale for Recommendations
CT is suggested as the initial imaging modality for non-pregnant adults with suspected diverticulitis due to its high diagnostic accuracy for diverticulitis. Additionally, CT can identify complications associated with diverticulitis (e.g., perforation, abscess, pylephlebitis, bowel obstruction, bleeding, fistula) and can be used to rule out other causes of abdominal pain.1,9-11 Compared to MRI, CT is more readily available, often more feasible, less costly, and may cause less distress for patients with a sensitivity to noise or confined spaces. Compared to US, obtaining a CT as the initial imaging test may decrease the need for additional imaging, resulting in saved time and resources. These benefits outweigh the risks attributed to CT of radiation exposure12,13 and contrast-associated side effects (e.g., contrast-induced nephropathy).
References
1. Expert Panel on Gastrointestinal Imaging: Weinstein S, Kim DH, Fowler, KJ, et al. ACR Appropriateness Criteria® left lower quadrant pain. Accessed October 3, 2023. https://acsearch.acr.org/docs/69356/Narrative/
2. Heverhagen JT, Sitter H, Zielke A, Klose KJ. Prospective evaluation of the value of magnetic resonance imaging in suspected acute sigmoid diverticulitis. Dis Colon Rectum 2008; 51(12): 1810-1815.
3. Lee IK, Jung SE, Gorden DL, et al. The diagnostic criteria for right colonic diverticulitis: prospective evaluation of 100 patients. Int J Colorectal Dis 2008; 23(12): 1151-1157.
4. Meyer S, Schmidbauer M, Wacker FK, Ringe KI. To fill or not to fill? - Value of the administration of positive rectal contrast for CT evaluation of diverticular disease of the colon. Rofo 2021; 193(7): 804-812.
5. Tomizawa M, Shinozaki F, Hasegawa R, et al. Abdominal ultrasonography for patients with abdominal pain as a first-line diagnostic imaging modality. Exp Ther Med 2017; 13(5): 1932-1936.
6. Toorenvliet BR, Bakker RF, Breslau PJ, Merkus JW, Hamming JF. Colonic diverticulitis: a prospective analysis of diagnostic accuracy and clinical decision-making. Colorectal Dis 2010; 12(3): 179-186.
7. van Randen A, Laméris W, van Es HW, et al. A comparison of the accuracy of ultrasound and computed tomography in common diagnoses causing acute abdominal pain. Eur Radiol 2011; 21(7): 1535-1545.
8. Weinrich JM, Bannas P, Avanesov M, et al. MDCT in the setting of suspected colonic diverticulitis: Prevalence and diagnostic yield for diverticulitis and alternative diagnoses. AJR Am J Roentgenol 2020; 215(1): 39-49.
9. Ferzoco LB, Raptopoulos V, Silen W. Acute diverticulitis. N Engl J Med 1998; 338(21): 1521-1526.
10. Wolfe C, Halsey-Nichols M, Ritter K, McCoin N. Abdominal pain in the emergency department: How to select the correct imaging for diagnosis. Open Access Emerg Med 2022; 14: 335-345.
11. Onur MR, Akpinar E, Karaosmanoglu AD, et al. Diverticulitis: A comprehensive review with usual and unusual complications. Insights Imaging 2017; 8: 19-27.
12. Shah KH, Slovis BH, Runde D, Godbout B, Newman DH, Lee J. Radiation exposure among patients with the highest CT scan utilization in the emergency department. Emerg Radiol 2013; 20(6): 485-491.
13. Sodickson A, Baeyens PF, Andriole KP, et al. Recurrent CT, cumulative radiation exposure, and associated radiation-induced cancer risks from CT of adults. Radiology 2009; 251(1): 175-184.
Recommendation: Diagnostic Imaging for Suspected Acute Diverticulitis (Pregnant People)
This recommendation is endorsed by the European Society of Clinical Microbiology and Infectious Diseases (ESCMID)
Section last reviewed and updated 06/13/2024
Last literature search conducted 10/22/2022
[View supplemental material here]
In pregnant adults with suspected acute diverticulitis, should CT, US (ultrasound), or MRI be obtained as the initial imaging modality?
Recommendation
In pregnant adults with suspected acute diverticulitis, US or MRI can be considered for imaging; however, the panel is unable to recommend one imaging modality versus the other (knowledge gap).
Results
We did not find any studies addressing diagnostic accuracy of imaging modalities for pregnant patients with suspected diverticulitis. However, we considered evidence from non-pregnant adults along with the balance between benefits and harms (e.g., radiation exposure) of each imaging modality.
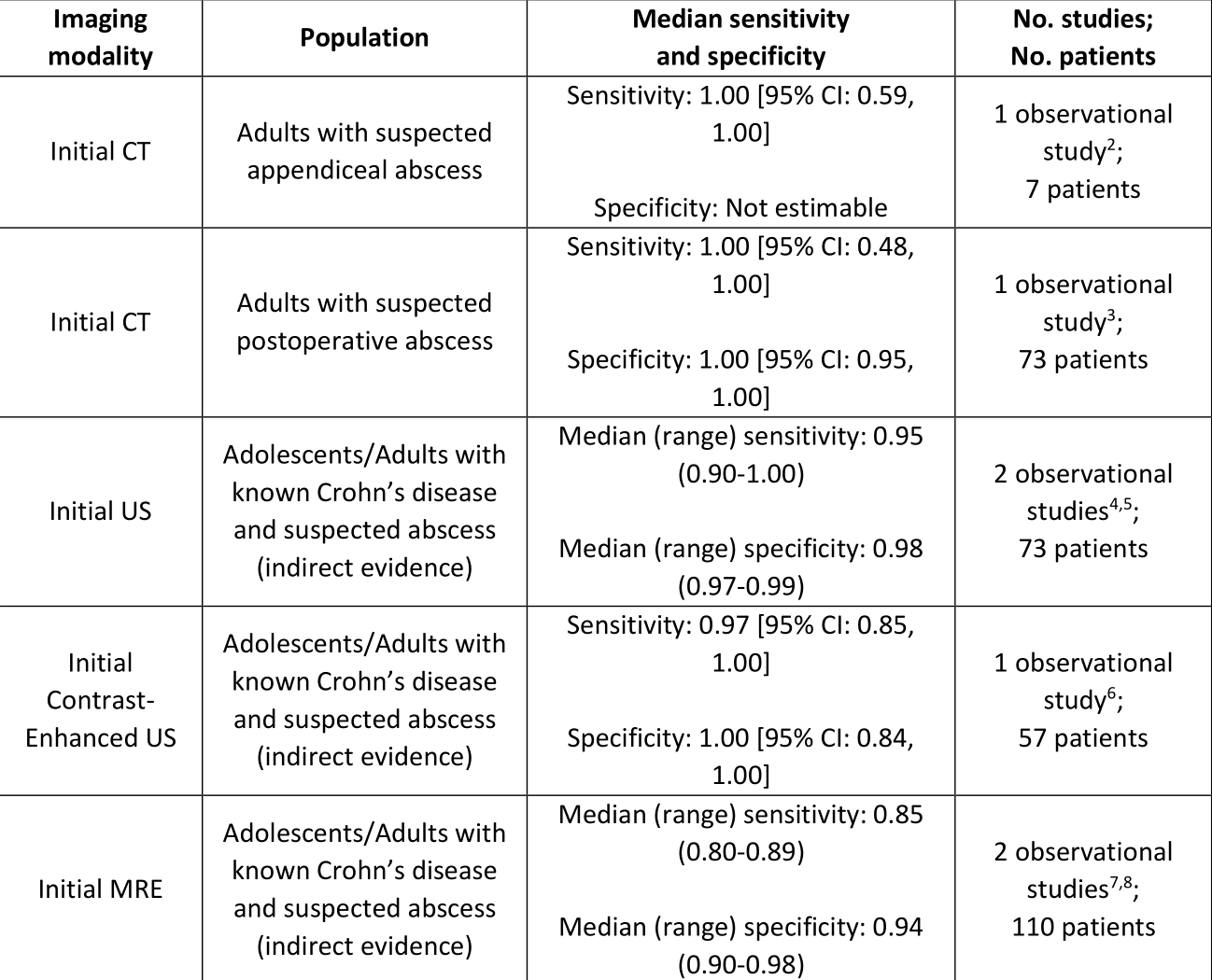
Recommendation: Diagnostic Imaging for Suspected Acute Intra-Abdominal Abscess (Adults)
This recommendation is endorsed by the European Society of Clinical Microbiology and Infectious Diseases (ESCMID) and the Pediatric Infectious Diseases Society (PIDS)
Section last reviewed and updated 06/13/2024
Last literature search conducted 10/22/2022
[View supplemental material here]
In adults with suspected acute intra-abdominal abscess, should abdominal US (ultrasound) or CT be obtained as the initial imaging modality?
In adults with suspected acute intra-abdominal abscess, if initial imaging is inconclusive, should MRI be obtained for subsequent imaging?
Recommendation
In non-pregnant adults and adolescents with suspected acute intra-abdominal abscess, we suggest obtaining an abdominal CT as the initial diagnostic imaging modality (conditional* recommendation, very low certainty of evidence).
Remarks
• When CT is obtained, the use of intravenous contrast may improve visualization of the abscess wall.1
• Because of CT’s accuracy, immediate additional imaging studies beyond CT should not be necessary.
*Conditional recommendations are made when the suggested course of action would apply to the majority of people with many exceptions, and shared decision-making is important.
Results
Seven observational studies2-8 were included in the analysis on whether to use CT, US, or MRI to identify acute intra-abdominal abscess in adults. Only one study2 addressed the sensitivity of CT in our patient population, i.e., patients with suspected acute intra-abdominal abscess; however, that study only included seven patients with intra-abdominal abscess. One additional study3 assessed diagnostic accuracy of CT for identifying five postsurgical intra-abdominal abscesses following bariatric surgery, and five studies were identified that addressed the diagnostic accuracy of US and MRE (magnetic resonance enterography) in adult and adolescent patients with Crohn’s disease with suspected intra-abdominal abscess.4-8
Summary of Evidence for Imaging Modalities Compared to Pathology for Diagnosing Acute Intra-Abdominal Abscess in Adults
Rationale for Recommendations
CT is suggested as the initial imaging modality for adults and adolescents with suspected acute intra-abdominal abscess due to its acceptable diagnostic accuracy for identifying intra-abdominal abscess. Since a large proportion of intra-abdominal abscesses develop postoperatively, a benefit of CT compared to US is its ability to maintain accuracy in the presence of dressings, stomas, or drains. Compared to US, CT is also less operator-dependent9,10 and less susceptible to decreases in accuracy when significant bowel gas is present, extensive surgical dressing or open wounds are in place, or with marked obesity.11 Potential harms of CT include radiation exposure, contrast-associated side effects (e.g., contrast-induced nephropathy), and unnecessary imaging in patients with no or equivocal CT findings.
References
1. Expert Panel on Gastrointestinal Imaging: Weinstein S, Kim DH, Fowler, KJ, et al. ACR Appropriateness Criteria® left lower quadrant pain. Accessed October 3, 2023. https://acsearch.acr.org/docs/69356/Narrative/
2. Kolb M, Storz C, Kim JH, et al. Effect of a novel denoising technique on image quality and diagnostic accuracy in low-dose CT in patients with suspected appendicitis. Eur J Radiol 2019; 116: 198-204.
3. Dupree A, de Heer J, Tichby M, et al. The value of CT imaging and CRP quotient for detection of postbariatric complications. Langenbecks Arch Surg 2021; 406(1): 181-187.
4. Allocca M, Fiorino G, Bonifacio C, et al. Comparative accuracy of bowel ultrasound versus magnetic resonance enterography in combination with colonoscopy in assessing Crohn's disease and guiding clinical decision-making. J Crohns Colitis 2018; 12(11): 1280-1287.
5. Neye H, Ensberg D, Rauh P, et al. Impact of high-resolution transabdominal ultrasound in the diagnosis of complications of Crohn's disease. Scand J Gastroenterol 2010; 45(6): 690-695.
6. Ripollés T, Martínez-Pérez MJ, Paredes JM, Vizuete J, García-Martínez E, Jiménez-Restrepo DH. Contrast-enhanced ultrasound in the differentiation between phlegmon and abscess in Crohn's disease and other abdominal conditions. Eur J Radiol 2013; 82(10): e525-e531.
7. Aaltonen G, Keranen I, Carpelan-Holmstrom M, Savolainen R, Linden R, Lepisto A. Intra-abdominal adhesions make the interpretation of magnetic resonance enterography in Crohn's disease more difficult. Dig Surg 2017; 34(1): 30-35.
8. Fallis SA, Murphy P, Sinha R, et al. Magnetic resonance enterography in Crohn's disease: a comparison with the findings at surgery. Colorectal Dis 2013; 15(10): 1273-1280.
9. Go HL, Baarslag HJ, Vermeulen H, Lameris JS, Legemate DA. A comparative study to validate the use of ultrasonography and computed tomography in patients with post-operative intra-abdominal sepsis. Eur J Radiol 2005; 54(3): 383-387.
10. Lin CM, Hung GU, Chao TH, Lin WY, Wang SJ. The limited use of ultrasound in the detection of abdominal abscesses in patients after colorectal surgery: compared with gallium scan and computed tomography. Hepatogastroenterology 2005; 52(61): 79-81.
11. Keller C, Wang NE, Imler DL, Vasanawala SS, Bruzoni M, Quinn JV. Predictors of nondiagnostic ultrasound for appendicitis. J Emerg Med 2017; 52(3): 318-323.
Recommendation: Diagnostic Imaging for Suspected Acute Intra-Abdominal Abscess (Children)
This recommendation is endorsed by the European Society of Clinical Microbiology and Infectious Diseases (ESCMID) and the Pediatric Infectious Diseases Society (PIDS)
[View supplemental material here]
In children with suspected acute intra-abdominal abscess, should abdominal US or CT be obtained as the initial imaging modality?
Recommendation
In children with suspected acute intra-abdominal abscess, we suggest obtaining an abdominal US as the initial diagnostic imaging modality (conditional* recommendation, very low certainty of evidence).
Remarks
• At least one study1 suggests MRI as a reasonable option for initial imaging of suspected acute intra-abdominal abscess in children.
• US is generally available but is also operator-dependent and can yield equivocal results. MRI is not always readily available, and sedation may be required for young children. CT is generally readily available but involves radiation exposure and may require use of IV contrast or sedation.
*Conditional recommendations are made when the suggested course of action would apply to the majority of people with many exceptions, and shared decision-making is important.
In children with suspected acute intra-abdominal abscess, if initial imaging is inconclusive, should MRI be obtained for subsequent imaging?
Recommendation
In children with suspected acute intra-abdominal abscess, if initial US is equivocal/non-diagnostic and clinical suspicion persists, the panel suggests either CT or MRI as subsequent imaging to diagnose acute intra-abdominal abscess (conditional* recommendation, very low certainty of evidence).
Remarks
• US is generally available but is also operator-dependent and can yield equivocal results. MRI is not always readily available, and sedation may be required for young children. CT is generally readily available but involves radiation exposure and may require use of IV contrast or sedation.
*Conditional recommendations are made when the suggested course of action would apply to the majority of people with many exceptions, and shared decision-making is important.
Results
Studies addressing diagnostic accuracy in children were not identified; however, a single comparative study addressing the utility of MRI vs. US to find a safe drainage pathway in children with a known or suspected appendiceal abscess was identified.1 A safe drainage pathway was identified in 86-98% vs. 75-81% of abdominal abscesses comparing MRI vs. US, respectively. When formulating recommendations for children, evidence for CT and MRI in adults was considered as indirect evidence.
Rationale for Recommendations
US is suggested as the initial imaging modality for children with suspected acute intra-abdominal abscess due to a slight preponderance of benefit vs. harm in comparison to either CT or MRI, as the panel placed a stronger weight on avoidance of radiation exposure and/or the need for sedation in children. However, when an intra-abdominal abscess is not observed on an US, but clinical suspicion persists, a low threshold should exist for performing a CT or MRI.
References
1. Abdeen N, Naz F, Linthorst R, et al. Clinical impact and cost-effectiveness of noncontrast MRI in the evaluation of suspected appendiceal abscesses in children. J Magn Reson Imaging 2019; 49(7): e241-e249.
Recommendation: Diagnostic Imaging for Suspected Acute Intra-Abdominal Abscess (Pregnant People)
This recommendation is endorsed by the European Society of Clinical Microbiology and Infectious Diseases (ESCMID)
[View supplemental material here]
In pregnant people with suspected acute intra-abdominal abscess, should abdominal US or MRI be obtained as the initial imaging modality?
Recommendation
In pregnant people with suspected acute intra-abdominal abscess, US or MRI can be considered as the initial diagnostic imaging modality; however, the panel is unable to recommend one versus the other (knowledge gap).
Results
No studies were found addressing diagnostic accuracy of imaging modalities for pregnant patients with suspected acute intra-abdominal abscess. Evidence is not yet available to establish a recommendation for pregnant people, though the panel agreed that either US or MRI would be appropriate. The panel considered evidence from non-pregnant adults, along with the balance between benefits and harms (e.g., radiation exposure) of each imaging modality.
Recommendation: Blood Cultures for Known or Suspected Intra-abdominal Infection (Adults and Children)
This recommendation is endorsed by the American Society of Microbiology (ASM), the European Society of Clinical Microbiology and Infectious Diseases (ESCMID), and the Pediatric Infectious Diseases Society (PIDS)
Section last reviewed and updated 06/13/2024
Last literature search conducted 10/22/2022
[View supplemental material here]
In adults and children with known or suspected intra-abdominal infection (uncomplicated or complicated), should blood cultures be obtained to effect a meaningful change in antimicrobial therapy?
Recommendation
In adults and children with suspected intra-abdominal infections who have an elevated temperature AND: hypotension and/or tachypnea and/or delirium, OR there is concern for antibiotic-resistant organisms that would inform the treatment regimen, we suggest obtaining blood cultures (conditional* recommendation, very low certainty of evidence).
Remarks
• Direct evidence on obtaining blood cultures in patients with intra-abdominal infections is lacking.
• Concern for antibiotic-resistant organisms includes high rates of regional resistance to commonly used agents administered as empiric treatment for intra-abdominal infections, patient history of any colonization or infection with organisms not susceptible to commonly used empiric regimens within the previous 90 days, antibiotic treatment within the previous 90 days, elderly or immunocompromised patients or patients with other significant comorbidities, and/or healthcare-associated infection.
*Conditional recommendations are made when the suggested course of action would apply to the majority of people with many exceptions, and shared decision-making is important.
Recommendation
In non-immunocompromised adults and children with suspected intra-abdominal infections who have a normal/elevated temperature but do not have hypotension, tachypnea, or delirium, and there is no concern for antibiotic-resistant organisms that would inform the treatment regimen, we suggest not routinely obtaining blood cultures (conditional* recommendation, very low certainty of evidence for adults/low certainty of evidence for children).
Remarks
• Direct evidence on obtaining blood cultures in patients with intra-abdominal infections is lacking.
• Clinicians should use their best judgment considering the benefits and risks of performing blood cultures. In select cases (e.g., concern for antibiotic-resistant organisms, concern for ascending cholangitis, complex intra-abdominal abscess), blood cultures may be helpful to assist with clinical decision-making and further management. Concern for antibiotic-resistant organisms includes high rates of regional resistance to commonly used agents administered as empiric treatment for intra-abdominal infections, patient history of any colonization or infection with organisms not susceptible to commonly used empiric regimens within the previous 90 days, antibiotic treatment within the previous 90 days, elderly or immunocompromised patients or patients with other significant comorbidities, and/or healthcare-associated infection.
Results
Seven observational studies1-7 were identified which addressed our prioritized outcomes of mortality and change in antimicrobial therapy. Only two of these studies3,7 were specific to patients with intra-abdominal infection. Other studies included a subset of patients with intra-abdominal infection in addition to patients receiving blood cultures for any other reason.
Summary of Evidence for Positive Blood Cultures as Predictors of Mortality and Meaningful Change in Therapy
*Change in antimicrobial therapy or management was defined differently across studies but generally included the initiation of antimicrobial therapy, change to appropriate antimicrobial therapy (narrowing, broadening, or optimizing regimen), lengthening treatment, or recalling patient for further assessment.
Rationale for Recommendations
The decision to obtain a blood culture should primarily be based on clinical suspicion of sepsis and criteria that require hospitalization and monitoring. Sensitive, but poorly specific, signs of sepsis include hypotension, tachypnea, and delirium. Blood culture yield is optimized when drawn prior to antimicrobial therapy. Collection of blood cultures should not be delayed while trying to discern whether hypotension responds to fluids or whether delirium is new-onset. Prediction models, such as the Shapiro prediction rule, have been developed as supplemental tools for emergency department physicians to improve blood culture utilization.8 However, these prediction models are not widely used and have not been robustly validated. Thus, the committee came to a consensus that using clinical signs and symptoms along with evidence from basic laboratory tests to determine who is at highest risk of sepsis can lead to more targeted utilization of resources than the use of prediction models.9 In addition, high rates of regional resistance to commonly used agents administered as empiric treatment for intra-abdominal infections or an individual patient’s known history of colonization or infection with organisms not susceptible to commonly used empiric regimens may warrant the collection of blood cultures.
References
1. Ehrenstein BP, Jarry T, Linde HJ, Scholmerich J, Gluck T. Low rate of clinical consequences derived from results of blood cultures obtained in an internal medicine emergency department. Infect, 2005; 33(5-6): 314-319.
2. Nakamura T, Takahashi O, Matsui K, Shimizu S, Setoyama M, Nakagawa M, et al. Clinical prediction rules for bacteremia and in-hospital death based on clinical data at the time of blood withdrawal for culture: an evaluation of their development and use. J Eval Clin Pract, 2006; 12(6): 692-703.
3. Otani T, Ichiba T, Seo K, Naito H. Blood cultures should be collected for acute cholangitis regardless of severity. J Infect Chemother. 2022; 28(2): 181-186.
4. Brown JD, Chapman S, Ferguson PE. Blood cultures and bacteraemia in an Australian emergency department: Evaluating a predictive rule to guide collection and their clinical impact. Emer Medicine Australasia, 2017; 29(1): 56-62.
5. Mountain D, Bailey PM, O’Brien D, Jelinek GA. Blood cultures ordered in the adult emergency department are rarely useful. Eur J Emerg Med, 2006; 13(2): 76-79.
6. Nishiyama M, Osawa K, Nakamura A, et al. The 24-h reporting of Gram stains from positive blood cultures contributes to physician's use of appropriate antimicrobials: Experience at a university hospital. J Infect Chemother. 2022; 28(6): 836-839.
7. Thompson GC, Morrison E, Ross M, Liu H, Vanderkooi OG, Eccles R. The use of routine blood cultures in pediatric appendicitis. Pediatr Emer Care, 2017; 33(12): e160-e163.
8. Shapiro N, Wolfe R, Wright S, Moore R, Bates D. Who needs a blood culture? A prospectively derived and validated prediction rule. J Emerg Med, 2008; 35(3): 255-264.
9. Evans L, Rhodes A, Alhazzani W, et al. Surviving Sepsis Campaign: International guidelines for management of sepsis and septic shock 2021. Crit Care Med. 2021; 49(11): e1063-e1143.
Recommendation: Intra-Abdominal Fluid Cultures for Known or Suspected Intra-abdominal Infection (Adults and Children)
This recommendation is endorsed by the American Society of Microbiology (ASM), the European Society of Clinical Microbiology and Infectious Diseases (ESCMID), and the Pediatric Infectious Diseases Society (PIDS)
Section last reviewed and updated 06/13/2024
Last literature search conducted 10/22/2022
[View supplemental material here]
In adults and children with known or suspected intra-abdominal infection (uncomplicated or complicated), should cultures of intra-abdominal fluid be obtained to effect a meaningful change in antimicrobial therapy?
Recommendation
In adults and children with complicated intra-abdominal infection who are having a procedure for source control, we suggest obtaining intra-abdominal cultures to guide antimicrobial therapy (conditional* recommendation, moderate certainty of evidence).
Remarks
• When obtaining intra-abdominal cultures, fluid inoculation is the preferred method of collection.
Recommendation
In adults and children with uncomplicated appendicitis undergoing an appendectomy, we suggest not routinely obtaining intra-abdominal cultures (conditional* recommendation, low certainty of evidence).
Remarks
• Immunocompromised patients are at increased risk for antibiotic-resistant organisms and intra-abdominal cultures are generally warranted.
• At the time of surgery, if complicated disease is suspected/recognized, intra-abdominal cultures may be advised.
*Conditional recommendations are made when the suggested course of action would apply to the majority of people with many exceptions, and shared decision-making is important.
Results
Eight observational studies examined how often peritoneal fluid culture results prompted a change in antimicrobial therapy in patients with complicated and/or uncomplicated appendicitis.1-8
Summary of Evidence for Obtaining Intra-Abdominal Cultures in Patients with Uncomplicated and/or Uncomplicated Intra-Abdominal Infection
*For all studies, change in antimicrobial therapy means a change to a different antimicrobial based on culture susceptibility results.
Rationale for Recommendations
For most patients with uncomplicated appendicitis, postoperative antibiotic therapy is not required, so obtaining a peritoneal fluid culture is unnecessary. Additionally, if a peritoneal fluid culture is obtained and incidentally positive (with no other signs/symptoms of infection), it may lead to unnecessary antimicrobial use.
For patients with complicated intra-abdominal infection, including complicated (perforated or gangrenous) appendicitis, positive peritoneal fluid cultures may provide useful information to guide antibiotic and/or antifungal selection. This is particularly true for patients who go on to fail therapy, experience a recurrence of infection, or are found to be infected with less common or multidrug-resistant microorganisms, including Candida spp. Additional benefits of targeted, narrow-spectrum therapy that is informed by culture data include the avoidance of drug-toxicity, C. difficile infections and exposure to broad-spectrum antibiotics that promote the emergence of antimicrobial resistance.
References
1. Tsuchiya A, Yasunaga H, Tsutsumi Y, Kawahara T, Matsui H, Fushimi K. Nationwide observational study of mortality from complicated intra-abdominal infections and the role of bacterial cultures. Br J Surg 2019; 106(5): 606-615.
2. Khan MN, Vidya R, Lee RE. Are routine peritoneal fluid cultures during appendicectomy justified? Ir J Med Sci 2007; 176(1): 37-40.
3. Tocchioni F, Tani C, Bartolini L, et al. The role of DNA amplification and cultural growth in complicated acute appendicitis. Pediatr Rep 2016; 8(3): 6487.
4. Viel-Theriault I, Bettolli M, Toye B, Harrison MA, Le Saux N. Contemporary microbiology and antimicrobial treatment of complicated appendicitis: The value of a short-term study. Pediatr Infect Dis J 2019; 38(11): e290-e294.
5. Wakeman D, Livingston MH, Levatino E, et al. Reduction of surgical site infections in pediatric patients with complicated appendicitis: Utilization of antibiotic stewardship principles and quality improvement methodology. J Pediatr Surg 2022; 57(1): 63-73.
6. Foo FJ, Beckingham IJ, Ahmed I. Intra-operative culture swabs in acute appendicitis: a waste of resources. Surgeon 2008; 6(5): 278-281.
7. Kenig J, Richter P. The need for culture swabs in laparoscopically treated appendicitis. Wideochir Inne Tech Maloinwazyjne 2013; 8(4): 310-314.
8. Moawad MR, Dasmohapatra S, Justin T, Keeling N. Value of intraoperative abdominal cavity culture in appendicectomy: a retrospective study. Int J Clin Pract 2006; 60(12): 1588-1590.