COVID 19: Reporting by clinical stages is needed for effective planning and response
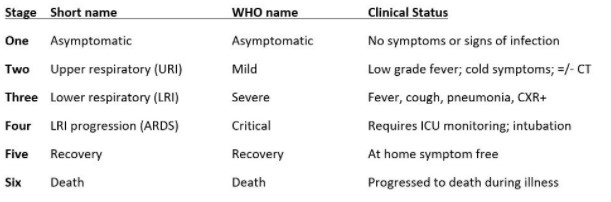
Facebook Twitter LinkedIn EmailCurrent clinical staging for the SARS-CoV2/COVID-19 pandemic can be divided into the six presentations below. All six require the presence of viral nucleic acid detected in respiratory secretions, but in China and soon in the United States and other nations, will include IgM/IgG antibody testing.
 The problem we are raising is that all these stages are aggregated and presented together as “total cases”.
The problem we are raising is that all these stages are aggregated and presented together as “total cases”.
What is missing and critical to our management of the pandemic in the United States is the distribution of how many at each stage is included in the overall case count in a region. Also lacking so far are analyses by standard demographic data such as residence, age, gender, and ethnicity. Such information is obviously critical for planning and managing resources such as PPE, isolation rooms, ICU beds and ventilators, for example. Likewise, planning treatment and prophylaxis trials will depend on knowing the location of eligible populations and their numbers.
For these reasons, we feel it is now time to consistently report the clinical stage of each COVID-19 patient following the WHO framework, above. This will allow comparison with other nations such as China, Italy, and many more, as the pandemic spreads across the Northern hemisphere and, soon escalates during the approaching winter in the Southern hemisphere. For example, asymptomatics are the most frequent type of “case” but have a much lower short-term rate of progression to criticality than severe cases.
It is equally critical to estimate the size of the recently infected asymptomatic population to assess the feasibility of contact-tracing and quarantine to limit spread. If this scheme is followed, the distributions of cases by stage will vary, but this is important in its own right in that jurisdictions can learn from each other based on their distribution and resultant outcome.
What is also missing is a population-based study of the natural history of COVID-19 in order to better understand and model the demands on the healthcare system over time, particularly the frequency and rates of progression of the disease through the various stages. Such studies performed in the early days of the AIDS pandemic gave invaluable information on the spectrum of disease and markers of progression to assist in the management of that outbreak. Although COVID-19 clearly differs in its routes of transmission and rapidity of clinical progression after infection, natural history data for COVID-19 could be similarly helpful for patient care, clinical trials, and resource allocation and planning. As it is, the question remains -- can one model the outcome of the pandemic in a region when the size and predicted fate of the largest group is largely unknown?


