Molecular HIV cluster detection shines a light on priority populations: Here’s how
Facebook Twitter LinkedIn Email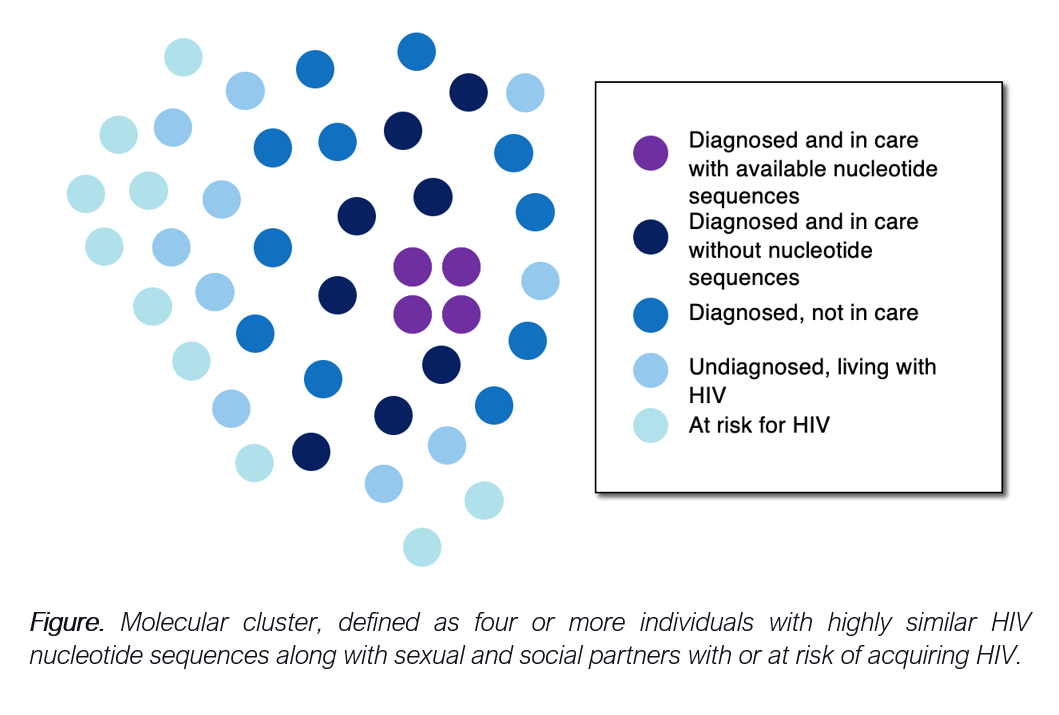 I was a first-year fellow in infectious diseases at Emory University, when my mentor, Dr. David Holland, called me in early 2021 asking me to support the Fulton County Board of Health’s response to several HIV molecular clusters. “OK! But ... what is an HIV molecular cluster?” was my first thought. Today, almost two years later, with new partnerships, and a recently formed Metro Atlanta Cluster Detection Response Team, I feel better prepared to discuss the topic.
I was a first-year fellow in infectious diseases at Emory University, when my mentor, Dr. David Holland, called me in early 2021 asking me to support the Fulton County Board of Health’s response to several HIV molecular clusters. “OK! But ... what is an HIV molecular cluster?” was my first thought. Today, almost two years later, with new partnerships, and a recently formed Metro Atlanta Cluster Detection Response Team, I feel better prepared to discuss the topic.
At diagnosis and throughout the HIV course, health care providers order a variety of tests, including HIV viral load, CD4 lymphocyte count and HIV drug-resistance testing. Through the latter, an HIV nucleotide sequence is obtained. Laboratories report back to the ordering provider to inform clinical care, and these tests are also securely shared with health departments conducting notifiable disease surveillance. HIV molecular clusters are detected using HIV nucleotide sequences.
Every month, HIV surveillance staff upload these sequences to a secure platform called HIV-Trace, where these are analyzed for similarities based on predetermined parameters, also known as the genetic distance threshold. Individuals who have experienced rapid HIV transmission have highly similar sequences and constitute a cluster. In Georgia, molecular clusters with four or more members diagnosed in the preceding 12 months are considered high priority. After detection, it is up to health departments to respond by addressing the gaps in services that contributed to rapid HIV transmission.
In 2018, the Centers for Disease Control and Prevention required all End the HIV Epidemic-funded districts to start responding to HIV clusters. Recent data suggest that these clusters grow at rates exceeding six times previously estimated national averages, highlighting the need to respond promptly. These responses include interventions at specific levels:
Cluster-specific responses refer to activities taken by health departments to assess the true extent of the cluster. Given that initially identified members of these clusters generally have entered HIV care and undergone drug-resistance testing through which a nucleotide sequence was obtained, these individuals only account for a portion of all cluster members (Figure). Health departments can conduct standard and enhanced partner services interviews with cluster members to identify sexual partners and social contacts who can benefit from HIV testing and subsequent referral to HIV treatment or preventive services. Unfortunately, many times these interviews provide limited information given the anonymous nature of sexual encounters or mistrust in public health entities. Further research is needed to evaluate innovative tools that could enhance partner reporting, engaging technology and culturally and linguistically competent approaches.
Member-specific responses are intended to ensure cluster members are receiving the medical and social services they need. Following a syndemic approach, cluster members should have an adequate follow-up with an HIV provider, and when needed, be offered mental health and substance use treatment, housing or financial assistance to address all the barriers that could interfere with HIV treatment adherence. Best practices to guide the implementation of member-specific responses are needed, including qualitative research informing how to approach cluster members with these services and assessing the impact of these activities on the HIV continuum of care.
Programmatic responses prioritizing individuals at risk of acquiring HIV. Addressing the gaps and tailoring HIV preventive services to communities at risk of experiencing rapid HIV transmission is essential. Identification of HIV clusters affecting Hispanic and Latino individuals has led to the expansion of culturally and linguistically concordant sexual health messaging in Fulton County, including social media ads highlighting access to HIV prevention and treatment regardless of insurance or immigration status. In several jurisdictions across the nation, molecular cluster detection has identified clusters among people who inject drugs, and responses have led to the implementation or expansion of syringe exchange programs. Similarly, clusters affecting primarily cis or transgender females should prompt health departments to assess resources and prioritize these communities.
Cluster detection and response in the state of Georgia
In early 2021, several HIV molecular clusters were detected in metropolitan Atlanta, primarily centered around gay and bisexual men and other men who have sex with men who identify as Hispanic or Latino. The Georgia Department of Public Health, in collaboration with CDC, conducted qualitative interviews with 65 service providers and 29 Hispanic and Latino gay and bisexual men to assess gaps and barriers to accessing medical and social services in metropolitan Atlanta. Overall language barriers were commonly mentioned, including widespread understaffing of bilingual providers at many levels and scarcity of educational materials in Spanish. Common structural barriers included lack of transportation, the inability of undocumented immigrants to obtain a driver's license in Georgia and fear of immigration or deportation repercussions when accessing services. When assessing HIV treatment and prevention barriers, participants mentioned issues navigating the U.S health care system.
Responding to these barriers, the Georgia Department of Public Health is developing a best practices document to aid organizations in the recruitment of bilingual staff. Health departments have developed educational materials in Spanish and launched media advertising for HIV prevention services in Spanish. To address issues navigating the health care system, Atlanta health departments have partnered with Emory University and two Latino-serving community-based organizations (Latino LinQ and Latino Community Fund – Georgia) and obtained federal funding to evaluate the implementation of an outreach campaign linking community members to a bilingual sexual health services navigator.
Health departments recognize advocacy groups’ apprehension regarding molecular cluster detection, raising concerns about the potential use of this information to criminalize people living with HIV. On the other hand, criminal law in Georgia was recently modernized to include considerations related to undetectable = untransmittable, and not disclosing HIV status is now considered a felony only if “intentional HIV transmission” is proven. Furthermore, the sequences collected through tools available to health departments cannot provide information on the directionality of transmission or provide information on whether links are direct or indirect. After a molecular cluster is identified, the main priority of health departments is addressing gaps in services and tailoring and prioritizing responses to communities and individuals with or at risk of HIV acquisition.
I have been tasked to lead the Metropolitan Atlanta Cluster Detection and Response Team efforts, and I believe the more tools we have to fight the HIV epidemic, the better care we will be able to provide to our priority populations. This opportunity has allowed me to collaborate with passionate leaders from community-based organizations and health departments, and I am convinced we have what it takes to end the HIV epidemic.
Related resources
- Georgia Department of Public Health, HIV Cluster Detection and Response
- CDC, HIV Cluster and Outbreak Detection and Response


