For antimicrobial stewardship training, ID fellows seek skills, not just knowledge
Facebook Twitter LinkedIn EmailAntimicrobial stewardship is emerging as a more integral component of infectious diseases practice given the rapidly increasing rates of antimicrobial resistance around the world. In light of this trajectory and the importance of safeguarding existing tools to combat infection, many ID trainees now consider what was once a niche subspecialization to be part and parcel of their overall training. However, recent studies suggest that current curricula are not meeting these needs, with only 50% of ID fellowship programs delivering formal antimicrobial stewardship content to their ID fellows. Compounding this lack of education is the little attention that has been paid to how ID fellows wish to receive this training.
This scarcity of research served as the impetus for our recent qualitative study, published in Clinical Infectious Diseases, exploring ID fellows’ recommendations regarding antimicrobial stewardship training. A total of 24 in-depth interviews were conducted with ID fellows across the United States to explore their experiences with and preferences for antimicrobial stewardship education during fellowship.
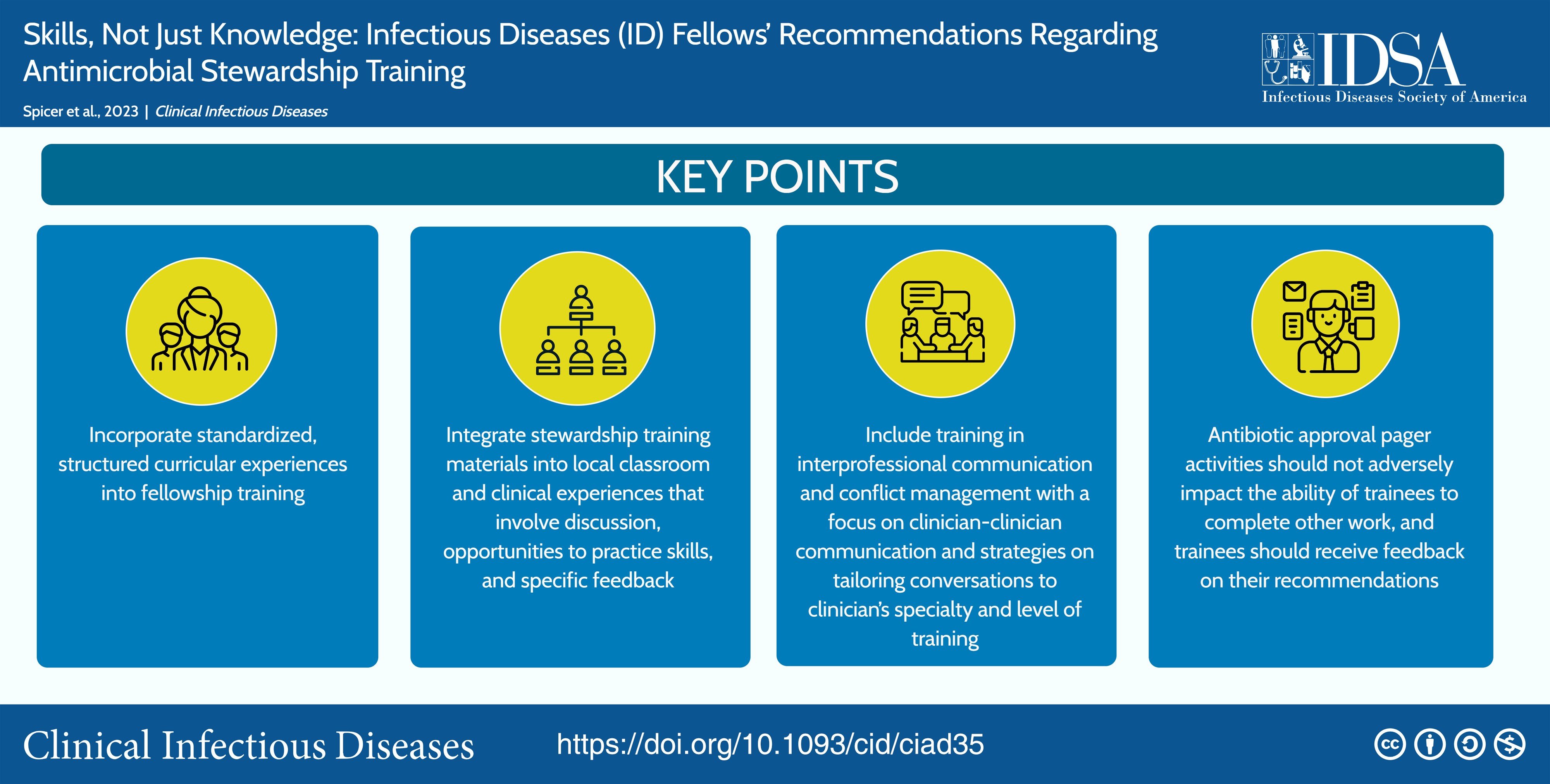
Several major themes emerged from descriptive, comparative and interpretive analysis of the data. First and foremost, participants reported that their experiences with antimicrobial stewardship were varied and largely informal. Many reported learning through “trial by fire,” an approach ultimately resulting in trainees with vastly different levels of stewardship knowledge and comfortability when delivering often contentious recommendations. There was an overwhelming desire for a standardized, in-person, practice-based curriculum to address this variability and ensure all fellows have equal knowledge of antimicrobial practices regardless of their place of training.
Additionally, formal training in interprofessional communication and conflict management was routinely requested so fellows could learn to “overturn objections” and “succinctly say why stewardship is so important.” Involvement of multidisciplinary faculty was seen as critical to achieving this aim, as other providers, such as surgeons, may offer different “pushback” not considered by ID attendings. Allowing practice in a safe space with sufficient feedback would facilitate improved communication across providers and specialties in the future. Importantly, fellows also emphasized the need to integrate this training with other curricula or otherwise ensure protected time so this additional instruction does not become overly burdensome.
In a post-pandemic era, there has never been more attention directed to the field of ID and the clear need for providers who are fully equipped to combat diseases capable of learning and adapting nearly as fast as we do. It is time that medical education does the same. The first and most critical step in this process is to explore the opinions and learning preferences of those most directly impacted — the trainees. Our study explored the perspectives of ID fellows and offered concrete solutions to bridge the gap in current stewardship curricula. Future research may build on this initial analysis to further improve upon these recommendations and better equip ID trainees to face the new and ever-changing challenges that are sure to lie ahead.
Visit the IDSA Academy website for more information about IDSA’s antimicrobial stewardship curricula for fellows.