From prescription to patient: The lifecycle of cabotegravir for PrEP
Facebook Twitter LinkedIn Email Long-acting injectable cabotegravir for HIV pre-exposure prophylaxis was approved by FDA in December 2021 (1), and the medication has been endorsed in several guidelines. (2-4) It’s considered a game changer for providers and organizations to serve certain populations in need of HIV prevention for which daily oral PrEP has been suboptimal. However, the number of current LAI CAB PrEP clients within health centers that already provide oral PrEP services has been relatively low nationwide.
Long-acting injectable cabotegravir for HIV pre-exposure prophylaxis was approved by FDA in December 2021 (1), and the medication has been endorsed in several guidelines. (2-4) It’s considered a game changer for providers and organizations to serve certain populations in need of HIV prevention for which daily oral PrEP has been suboptimal. However, the number of current LAI CAB PrEP clients within health centers that already provide oral PrEP services has been relatively low nationwide.
While several factors contribute to the slow prescribing and implementation uptake, such as low provider and community awareness and low organizational capacity, it’s also important to focus on the evolving and heterogeneous nature of insurance company responses to paying for LAI CAB PrEP after a prescription is written by a licensed medical provider. We write to share our experiences with what happens after an LAI PrEP prescription is written, how insurance companies have responded and how their responses complicate our conversations with potential seekers of LAI CAB PrEP. We want to inform other health care professionals and leaders so they are further equipped in their fight for equitable access to this PrEP medication.
The maze of insurance coverage & payment policies
Once a prescription is issued, it sets off a chain of processes, typically carried out by multiple health staff members, such as pharmacists or navigators, at clinics. One of the essential first steps is to forward the prescription to the person’s insurance company to confirm they will cover the cost of the medication before giving it to the patient or sending it to the pharmacy.
 The feedback from the insurance company generally falls into several categories (5), outlined in Table 1, although these are not exhaustive — it’s complicated!
The feedback from the insurance company generally falls into several categories (5), outlined in Table 1, although these are not exhaustive — it’s complicated!
In addition, to be eligible for the medical benefit, some insurance companies require proof of a recent HIV RNA test as well as proof of documentation within the medical record that the client “failed” two other forms of prevention. Some examples of language we have received in letters from insurance companies are highlighted in Table 2.
The impetus behind this blog post is the challenges associated with medical benefits with no guaranteed payment (see category #3 in Table 1). This process generally requires the medication to be purchased upfront at some risk to the clinic and patient. The cost is reimbursed to the purchaser, typically a health clinic, contingent on meeting all reimbursement criteria set by the insurance provider and AFTER the client receives the injection.
One quandary arising from this “medical benefit” approach is the vagueness and inconsistency of the documentation criteria among different insurance companies. Meeting these criteria often demands a considerable amount of staff time and effort to secure reimbursements.
The “no guaranteed” payment clause presents health centers with a financial predicament. Who will bear the cost of the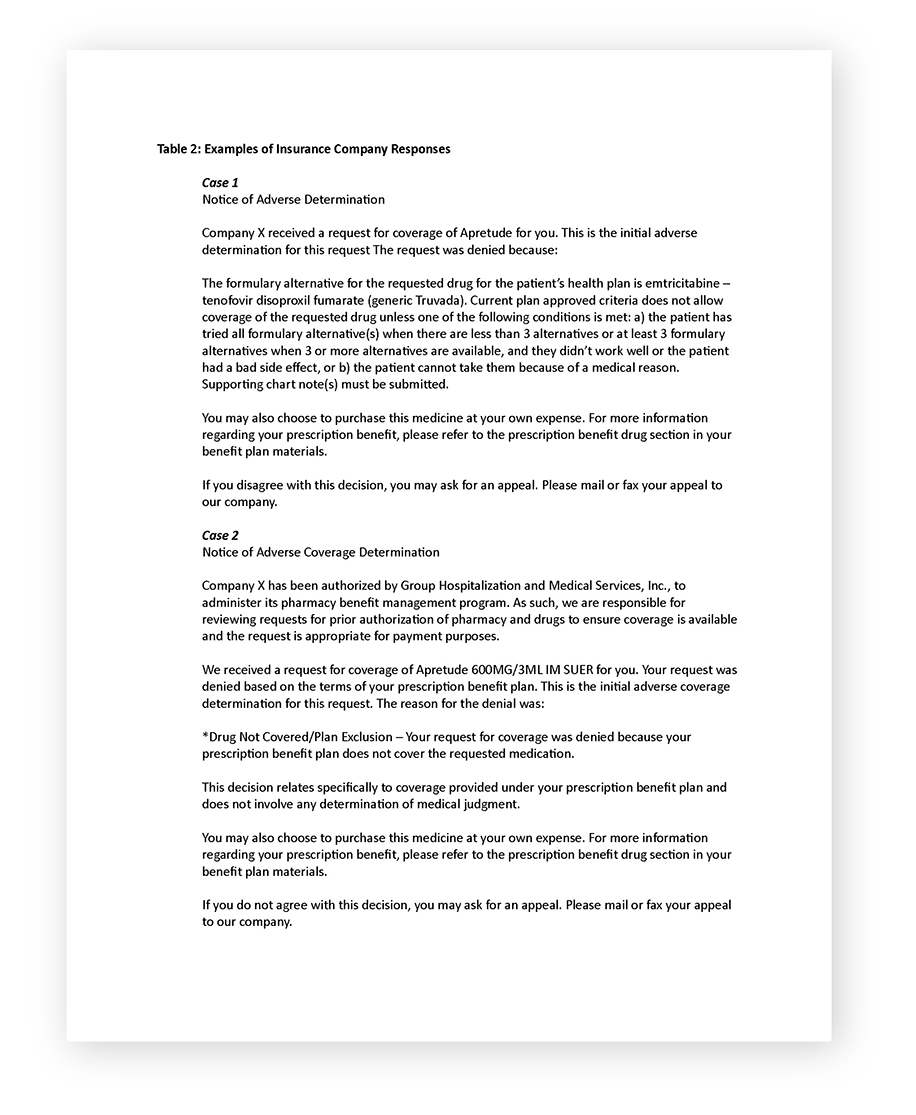 medication if the reimbursement does not come through after its administration? Who or what organization can afford to take on this financial risk of administering the medication? How can we reasonably expect a client to shoulder 100% of this risk?
medication if the reimbursement does not come through after its administration? Who or what organization can afford to take on this financial risk of administering the medication? How can we reasonably expect a client to shoulder 100% of this risk?
The patient-provider relationship
Furthermore, how do we as health care providers delicately yet transparently communicate to our clients seeking LAI CAB PrEP about the health center’s inability to undertake such a risk? This complexity presents a challenging situation that necessitates immediate attention and innovative solutions.
The escalating complexity of declarations coming from insurance companies, particularly commercial ones, paints a disturbing picture. Given that two-thirds of Americans are covered by commercial or non-public insurance (6), the impact of this situation is far-reaching. We are seeing these insurance companies introduce clauses that induce fear among medical organization leaders over potential risks, a fear that might come at a staggering cost — thousands of dollars per LAI CAB PrEP user and, in the aggregate, hundreds of thousands of dollars for multiple PrEP users. (7, 8)
The cost of innovation
Injectable cabotegravir for HIV prevention costs approximately $3,700 per injection, and seven such injections are recommended per year. This considerable expenditure is giving rise to a pressing question: With the continually shifting insurance landscape, will clients initiate LAI CAB PrEP, only to have to transition off due to complex coverage and reimbursement issues?
The crux of these dilemmas goes to the heart of the sustainability of LAI CAB PrEP programs. Unlike with generic oral PrEP delivery, both organizations and clients are heavily reliant on funding from insurance companies. This dependency is causing a significant strain on the system. The process has overburdened clinic staff and other health workers, resulted in extended wait times for LAI CAB PrEP initiation, and, perhaps most distressingly, led to confusion and inconsistent communication regarding access to this medication.
These coverage challenges, payment issues and the question of “who shoulders the financial risk” — and the constant back-and-forth that occurs behind the scenes during LAI CAB PrEP prescribing — all will play an instrumental role in determining the future of this innovative intervention. If we are to scale up and optimize the use of LAI CAB PrEP to protect individuals at risk for HIV, we must confront and overcome these challenges. To win this fight against HIV, the clarity, efficiency and affordability of the process is paramount. It’s high time to address these issues by requiring insurers to cover all forms of PrEP and unlock the potential of this innovation.
For more information, including de-identified insurance denial letters, please contact Rupa R. Patel, MD, MPH.
References
- U.S. Food and Drug Administration. FDA Approves First Injectable Treatment for HIV Pre-Exposure Prevention. Available at: https://www.fda.gov/news-events/press-announcements/fda-approves-first-injectable-treatment-hiv-pre-exposure-prevention. [Accessed May 17, 2023].
- U.S. Public Health Service. Preexposure prophylaxis for the prevention of HIV infection in the United States—2021 Update: a clinical practice guideline. Available at: https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2021.pdf. Published 2021. [Accessed May 17, 2023].
- Gandhi RT, Bedimo R, Hoy JF, et al. Antiretroviral Drugs for Treatment and Prevention of HIV Infection in Adults: 2022 Recommendations of the International Antiviral Society–USA Panel. JAMA. 2023;329(1):63–84. doi:10.1001/jama.2022.22246
- Guidelines on long-acting injectable cabotegravir for HIV prevention. Geneva: World Health Organization; 2022. License: CC BY-NC-SA 3.0 IGO.
- National Association of Medication Access & Patient Advocacy, Inc. The Importance of a Thorough Benefits Investigation to Help Navigate Medical vs Pharmacy Benefit. Available at: https://namapa.org/medical-vs-pharmacy-benefit. [Accessed: May 17, 2023].
- U.S. Census Bureau. American Community Survey Tables for Health Insurance Coverage 2021. American Community Survey. Available at: https://www.census.gov/data/tables/time-series/demo/health-insurance/acs-hi.html. [Accessed: May 17, 2023].
- Cains G. Injectable PrEP can only cost a little more than oral PrEP if it is to be cost-effective, South African study finds. Available at: https://www.aidsmap.com/news/aug-2022/injectable-prep-can-only-cost-little-more-oral-prep-if-it-be-cost-effective-south#:~:text=Not%20counting%20overheads%2C%20at%20high,injection%20(%2490%20a%20year). [Accessed May 17, 2023].
- Jamieson L et al. (presenter Meyer-Rath G) The relative cost-effectiveness of long-acting injectable cabotegravir versus oral pre-exposure prophylaxis: a modelled economic evaluation and threshold analysis in South Africa based on the HPTN 083 and 084 trials. 24th International AIDS Conference, Montreal, abstract OAE0304, 2022.
Potential conflicts of interest: Dr. Patel receives research funding from Gilead Sciences Inc. and ViiV Healthcare. Dr. Khan receives research funding from ViiV Healthcare. Drs. Nunn and Chan report no potential conflicts.


