Pneumocystis jirovecii pneumonia in severe alcohol-associated hepatitis: A call for prophylactic action
Facebook Twitter LinkedIn Email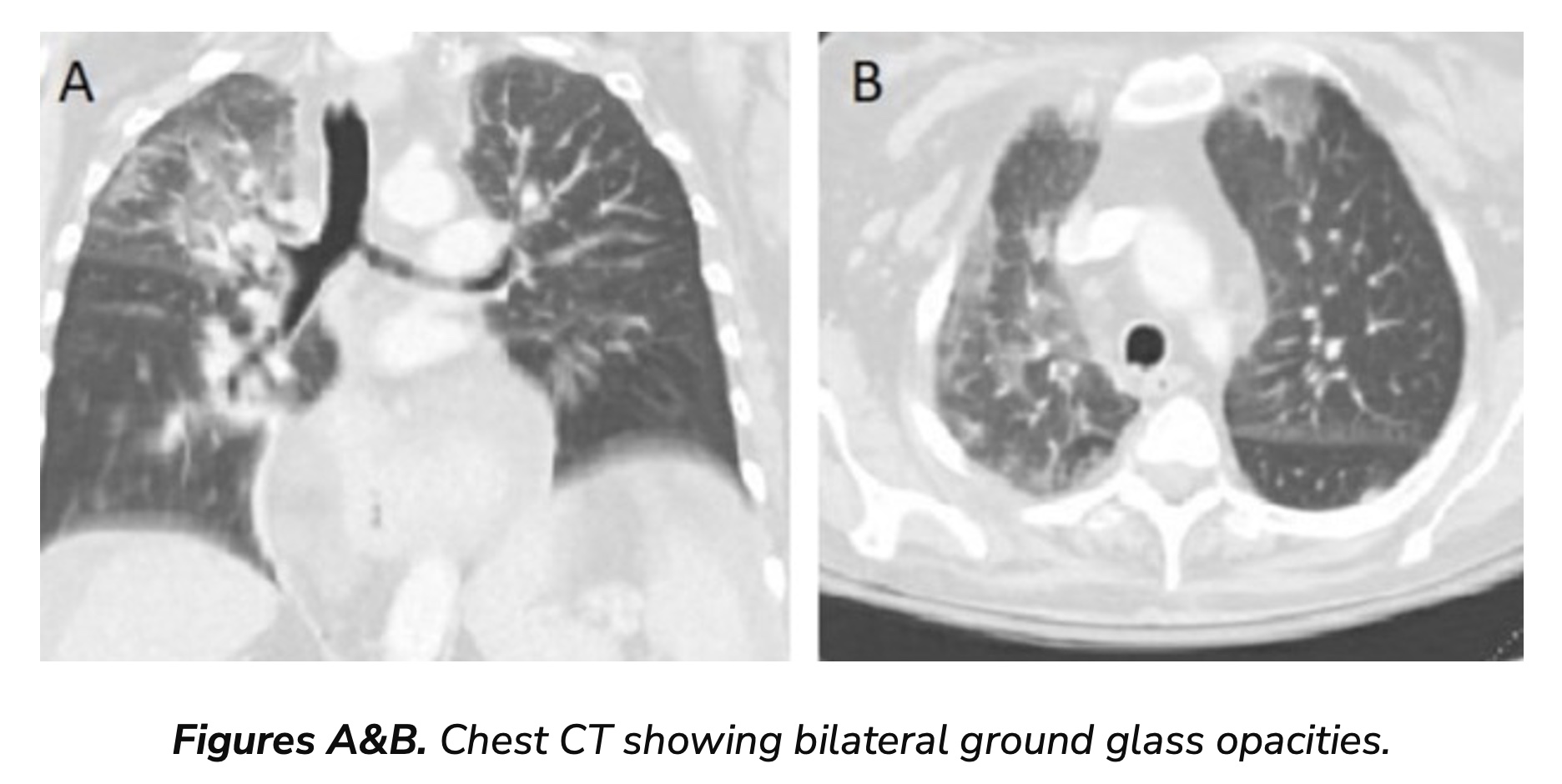 Pneumocystis jirovecii pneumonia is a formidable threat to immunocompromised people, primarily associated with HIV infection. However, recent research underscores the alarming incidence of PJP in non-HIV immunosuppressed patients, particularly those with severe alcohol-associated hepatitis. Despite the growing recognition of this risk, there remains a significant gap in clinical consensus regarding PJP prophylaxis in AAH patients. (1)
Pneumocystis jirovecii pneumonia is a formidable threat to immunocompromised people, primarily associated with HIV infection. However, recent research underscores the alarming incidence of PJP in non-HIV immunosuppressed patients, particularly those with severe alcohol-associated hepatitis. Despite the growing recognition of this risk, there remains a significant gap in clinical consensus regarding PJP prophylaxis in AAH patients. (1)
In a landmark article published in JAMA by Zhou et al. in June 2023, recommendations were outlined for PJP prophylaxis in non-HIV immunocompromised adults. (2) The recommendations stipulated that patients receiving high-dose corticosteroids, equivalent to or exceeding 20 mg of prednisone daily for at least one month, along with an additional cause of immunodeficiency, should receive PJP prophylaxis. However, the definition of this additional immunosuppressive state remained ambiguous, leaving a critical void in clinical practice.
According to the 2022 National Survey on Drug Use and Health, conducted by the Substance Abuse and Mental Health Services Administration, an estimated 29.5 million people in the U.S. aged 12 and older had alcohol use disorder, with roughly 20% of those individuals estimated to have AAH, with or without cirrhosis. The dysregulation induced by alcohol and its metabolites creates a milieu conducive to infections. The mechanism is considered secondary to these metabolites causing a compromise in the integrity of cell junctions of the digestive tract, leading to heightened intestinal permeability. This, in turn, allows for an increased influx of lipopolysaccharide, dysregulating the inflammatory pathways through toll-like receptors. Furthermore, alcohol consumption has been shown to impact antigen presentation and the function of CD4+ and CD8+ cells, further predisposing heavy drinkers to infections. (3,4)
In the management of such severe AAH, where patients are often administered high doses of prednisolone, the risk of PJP pneumonia becomes a concerning reality. This has been previously evidenced by several clinical cases and emerging research. (5,6)
We had a tragic case highlighting this critical need to prioritize PJP prophylaxis in AAH. The patient, an adult over the age of 60, was initially managed for severe AAH with high-dose steroids and later was admitted following a fall and rapid clinical deterioration. This patient developed acute hypoxic respiratory failure requiring mechanical ventilation. The chest imaging was consistent with bilateral diffuse opacities in the lung fields. (Figures A&B) No overt cause of respiratory failure was determined. Infectious workup was unrevealing for bacterial causes while the patient remained on broad-spectrum antibiotics. Due to refractory hypoxemia and multi-organ failure with shock, the patient was transitioned to comfort care. Two days after the patient died, the bronchial alveolar lavage revealed a positive PCR for PJP. Unfortunately, it was too late for any meaningful intervention.
While the debate on use of antibacterial prophylaxis in severe AAH has been settled with some studies, including Louvet et al. (7), the question of PJP prophylaxis remains unanswered. (5) Considering the heightened susceptibility of AAH patients to infections, particularly after steroid use, proactive measures are imperative to prevent worse outcomes like in the case of our patient. Health care providers should recognize the immunosuppressive nature of AAH and consider PJP prophylaxis as a standard of care.
References
- Kovacs JA, Hiemenz JW, Macher AM, et al. Pneumocystis carinii pneumonia: a comparison between patients with the acquired immunodeficiency syndrome and patients with other immunodeficiencies. Ann Intern Med. 1984;100(5):663-671. doi:10.7326/0003-4819-100-5-663
- Zhou S, Aitken SL. Prophylaxis Against Pneumocystis jirovecii Pneumonia in Adults [published correction appears in JAMA. 2023 Oct 3;330(13):1289]. JAMA. 2023;330(2):182-183. doi:10.1001/jama.2023.9844
- Kaur B, Rosenblatt R, Sundaram V. Infections in Alcoholic Hepatitis. J Clin Transl Hepatol. 2022;10(4):718-725. doi:10.14218/JCTH.2022.00024
- Pasala S, Barr T, Messaoudi I. Impact of Alcohol Abuse on the Adaptive Immune System. Alcohol Res. 2015;37(2):185-197.
- Faria LC, Ichai P, Saliba F, et al. Pneumocystis pneumonia: an opportunistic infection occurring in patients with severe alcoholic hepatitis. Eur J Gastroenterol Hepatol. 2008;20(1):26-28. doi:10.1097/MEG.0b013e3282f16a10
- Franceschini E, Dolci G, Santoro A, et al. Pneumocystis jirovecii pneumonia in patients with decompensated cirrhosis: a case series. Int J Infect Dis. 2023;128:254-256. doi:10.1016/j.ijid.2022.12.027
- Louvet A, Labreuche J, Dao T, et al. Effect of Prophylactic Antibiotics on Mortality in Severe Alcohol-Related Hepatitis: A Randomized Clinical Trial. JAMA. 2023;329(18):1558-1566. doi:10.1001/jama.2023.4902


