Syphilis surge: The great imitator strikes again
Facebook Twitter LinkedIn Email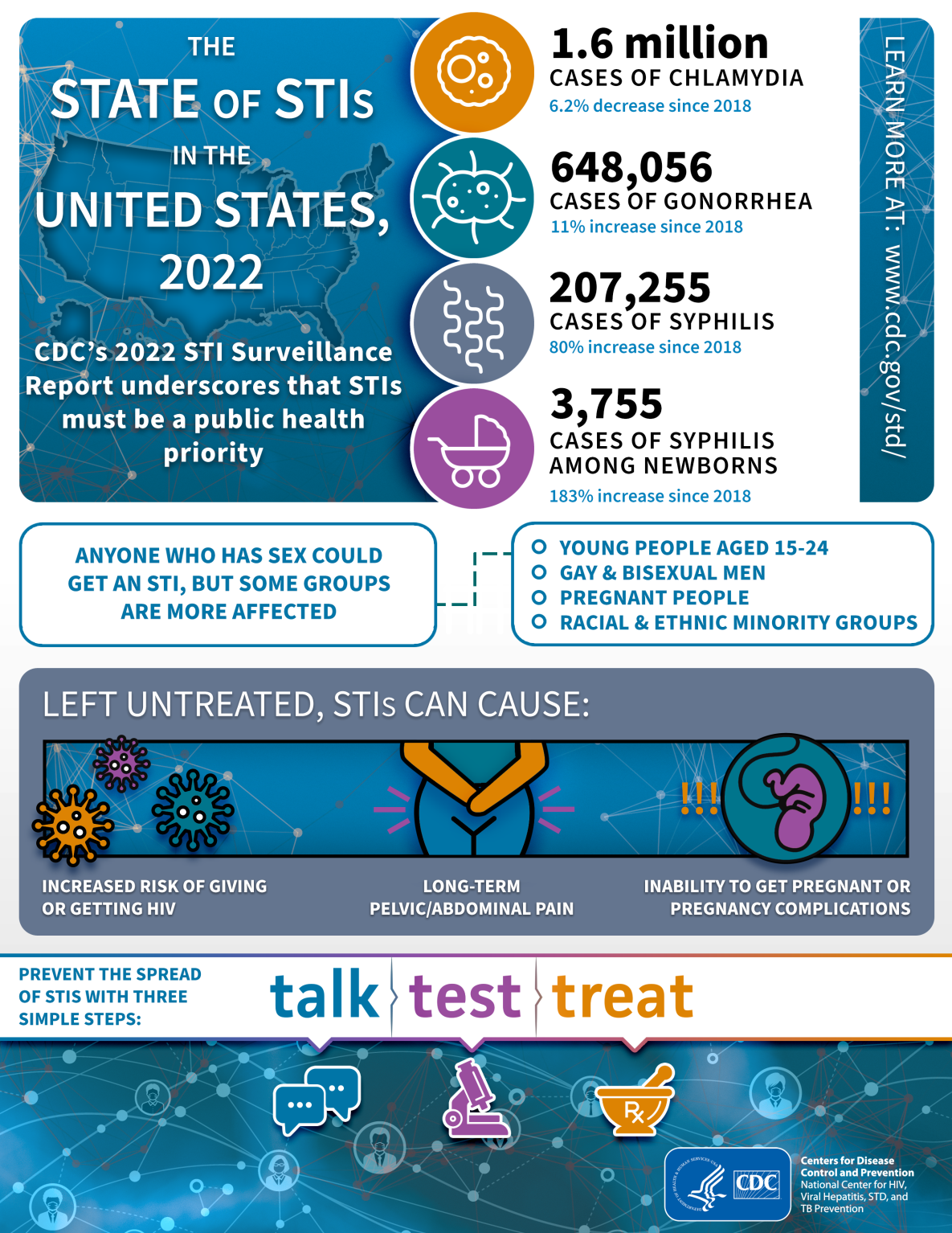 In late January, the Centers for Disease Control and Prevention confirmed what many of us who provide care for people with sexually transmitted infections already knew: We are in the midst of a surge in syphilis cases. How big is the surge exactly? Between 2018 and 2022, syphilis cases increased 80% with a total of 207,255 cases of primary and secondary syphilis reported in the U.S. in 2022. Even more startling is the rise in the cases of congenital syphilis, which totaled 3,755 in 2022, a 183% increase since 2018. (1)
In late January, the Centers for Disease Control and Prevention confirmed what many of us who provide care for people with sexually transmitted infections already knew: We are in the midst of a surge in syphilis cases. How big is the surge exactly? Between 2018 and 2022, syphilis cases increased 80% with a total of 207,255 cases of primary and secondary syphilis reported in the U.S. in 2022. Even more startling is the rise in the cases of congenital syphilis, which totaled 3,755 in 2022, a 183% increase since 2018. (1)
Now let’s put this into perspective: Few people in training now likely know that in the year 2000, we had only 5,789 cases of primary and secondary syphilis, representing an all-time low. (2) CDC at the time had a Syphilis Elimination Effort. (3) Yes, that is right — we were near eliminating syphilis in the U.S. in the early 2000s, and now we are seeing the highest rates since the 1950s.
In my STI clinic in St. Louis County in Missouri, the words “You’ve got to be kidding me!” are often said when syphilis titers come back positive for a patient where there was no suspicion of syphilis during the clinical encounter. Whenever one of my trainees says they have never seen a syphilis case, I laugh on the inside and think to myself, “Oh, yes, you have, you just didn’t know it!” I don’t blame any trainee or colleague for thinking that way, as there is a whole generation of clinicians who have never seen syphilis before. Remember, we were near elimination 20 years ago. Now, if you’re lucky enough to rotate in my clinic, or with one of my brilliant STI colleagues across the U.S., you will certainly see more syphilis than you ever thought possible and be humbled by the many ways “the great imitator” can appear. In my clinic, there is no rash that goes without syphilis testing, and you will often hear me call out to my colleagues whenever they are discussing a case, “Could it be syphilis?” Most commonly the answer is, “Well, it could be!”
Once the syphilis statistics from CDC came out earlier this year, everyone asked why cases had surged. Are people having more sex? Not sure. Are people using condoms less? Most certainly; condoms were never really popular to begin with. Are people on HIV PrEP to blame? First off, never blame people for their sex lives and for taking control of their sexual health. Secondly, individuals on PrEP get tested every 3 months for bacterial STIs and HIV, which means they are more likely to detect asymptomatic cases — isn’t that what we want? What about dating apps? They’ve been around for around 20 years, but we must remember correlation does not mean causation.
Here’s what I believe are the largest reasons for the spread of syphilis and other STIs: The combination of years of an underfunded public health sector, especially STI clinics, combined with back-to-back pandemics. Federal funding for STI clinics has remained stagnant, state funding has decreased, and — taking inflation into consideration — our public health sector is hurting. (4) We see this reality reflected in every health department we visit as part of the National Network of STI/HIV Prevention Training Centers. Also, according to CDC, STI detection dropped during the pandemic, with 91% of jurisdictions reporting that in April 2020, staff reassignment to COVID-19 work had moderate to great impact on their work. Fifty-three percent of jurisdictions reported discontinuing disease intervention specialists’ field work, and 28% reported permanent reassignment of these specialists to COVID-19 duties. (5,6)
These specialists are specifically tasked with doing contact tracing for HIV and syphilis in most health departments, ensuring individuals and their sexual partners get tested and treated appropriately. After COVID-19, mpox hit, and once again, STI clinics were tasked with another disease outbreak, dealing with testing, treatment and vaccination efforts. And then we had a benzathine penicillin G shortage that started last year and continues today, leading many health departments to not have the first-line treatment for syphilis in stock. Back-to-back pandemics, high staff turnover, reassigned resources, lack of treatment access and burnout have created a perfect storm leading to the surge we are currently seeing.
So what can as health care providers and public health advocates do? Adequately fund STI clinics and disease intervention specialists’ services with stable funding. Utilize your Prevention Training Centers (find out more at nnptc.org) to train your staff and clinicians. Know that, as a health care provider, there is always an expert you can submit your questions to via stdccn.org, a virtual clinical consultation network. Normalize talking about sexual health as part of every clinical encounter to decrease stigma and increase acceptance of testing and services. Batch STI tests, making sure that when you are testing for HIV, you are also testing for chlamydia, gonorrhea (especially extragenital sites if your patients are having oral or anal sex) and syphilis all together. And become familiar with the ever-evolving face of syphilis, because if it isn’t in the differential, it won’t be tested for.
References
- Centers for Disease Control and Prevention. Sexually Transmitted Infections Surveillance, 2022. Atlanta: U.S. Department of Health and Human Services; 2024.
- Syphilis Rate Declines to ALL-TIME LOW in 2000. Centers for Disease Control and Prevention.
- Syphilis Elimination Effort (SEE). Centers for Disease Control and Prevention.
- STI Economics, Public-Sector Financing and Program Policy. In: Sexually Transmitted Infections: Adopting a Sexual Health Paradigm. National Academies of Sciences, Engineering and Medicine; Health and Medicine Division; Board on Population Health and Public Health Practice; Committee on Prevention and Control of Sexually Transmitted Infections in the United States; Crowley JS, Geller AB, Vermund SH, eds. Washington, D.C.: National Academies Press (U.S.); 2021 March 24.
- Sexually Transmitted Infections Surveillance, 2022 – Technical Notes: Impact of COVID-19 on STIs. Centers for Disease Control and Prevention.
- How the COVID-19 Pandemic Has Impacted Sexually Transmitted Diseases (STD) Programs. Centers for Disease Control and Prevention.


